The health scheme is scheduled to be functioning by 2025 but the precise costs are still not known.
NEWS ANALYSIS
In just 10 years from now, South Africans could be paying significantly less for private health services; spending an entire day at a public clinic waiting to see a doctor – if at all – will be a thing of the past and there will be no more out-of-pocket payments for medication or treatment.
This is the healthcare system envisioned in the recently published National Health Insurance (NHI) white paper, which provides a detailed plan of reforms in both the public and private sectors to make affordable, good-quality healthcare accessible to all South Africans.
The implementation of the NHI is likely to be politically controversial, as have similar far-reaching overhauls of health systems in other countries. But South Africa is following a well-blazed path, and one with much multilateral backing, such as:
- A 2005 World Health Organisation member states (including South Africa) commitment to ensuring that “all people have access to health services they need without risk of financial ruin or impoverishment”;
- A 2012 United Nations resolution urging governments around the world to move towards universal health coverage; and
- The inclusion of universal health coverage in the sustainable development goals.
Countries such as Brazil, Norway and Mexico have similar systems in place. The results have been largely positive.
Economic gain
Research indicates that middle-income countries, such as South Africa, that are implementing NHI-type systems have benefited from a healthier population. The white paper estimates that “a one-year increase in a nation’s average life expectancy can increase GDP [gross domestic product] per capita by 4% in the long run”.
In South Africa, only 16% of the population belong to medical aid schemes and have access to private medical treatment. The remainder of the population depend on the public sector for health services, which are often of a much poorer quality.
Speaking at the release of the white paper, Health Minister Aaron Motsoaledi said “the existence of medical schemes in South Africa is a punishment for poor people” because 80% of the specialists in South Africa work in the private sector where they treat only 16% of the population – about eight million people.
Motsoaledi also pointed out that health service prices in South Africa are very close to those of the United States, which has the most expensive healthcare system in the world.
Although it has taken four years since the publication of the green paper for the NHI white paper to be released, and we still don’t know exactly how this will be financed, the health department is determined to introduce the scheme.
Phased in
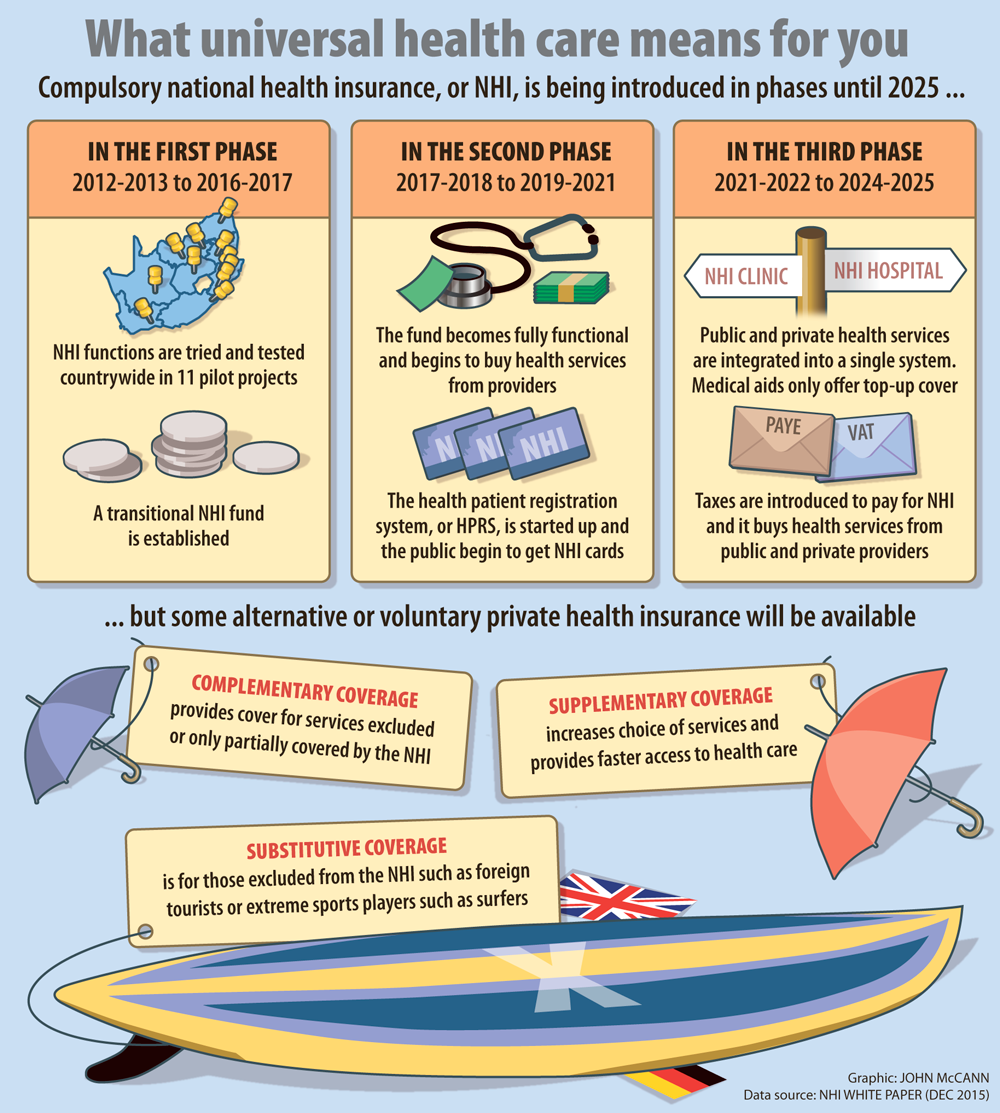
The NHI is being implemented over a 14-year period, which will be divided into three phases. The first, which started in 2012 and is due to run until 2017, will see the NHI “tested” in 11 health districts. The main focus of the pilot scheme is to fix the system and lay the foundation for the NHI.
Since 2012, several reforms have taken place, such as the introduction of the integrated school health programme, district clinical specialist teams and the establishment in 2013 of the office of health standards compliance. More than 300 private general practitioners have been contracted to work in government clinics in the pilot districts. But there is still a lot of work to be done, especially in the NHI pilot districts, where there are still reports of systemic failures.
The second phase, which is due to take place over five years between the 2017-2018 and 2019-2021 financial years, will see funds from the Compensation Fund and the Road Accident Fund being redirected to the NHI Fund.
Subsidies paid to medical schemes by government departments will also be allocated to the fund, which is due to be fully functional by end of this phase. The registration process for people who will be covered by the NHI will start in this phase, with “vulnerable groups” given priority.
The third and final phase will take place over four years, between the 2021-2022 and 2024-2025 financial years, when a mandatory contribution in the form of taxes will be enforced.
The NHI Fund will contract private hospitals and specialists to provide services where the government is unable to. By 2025, medical aids will only provide top-up cover to pay for services such as elective cosmetic surgery that will not be paid for by the NHI.
Single system
When the scheme is in full swing there will be only one health system.
By using their NHI card, South Africans will be able to access health services from any doctor or clinic, public or private, that is certified and accredited by the NHI.
The scheme will provide a “comprehensive” package of health services, but it will not cover everything for everyone. All healthcare will be provided at the primary healthcare level, and hospitals and specialists will only be for referral.
Though it is yet to be finalised, the basic NHI package will cover the following services: HIV and tuberculosis, reproductive healthcare, optometry and mental health.
Implementing reform on this scale is a mammoth task, which requires skills, resources and leadership. The popular, effective and politically well
-capitalised Motsoaledi has made considerable progress, but has yet to secure the buy-in of the private sector and the guarantees of the additional funding required.
In policy terms, 2025 is not all that far away.
