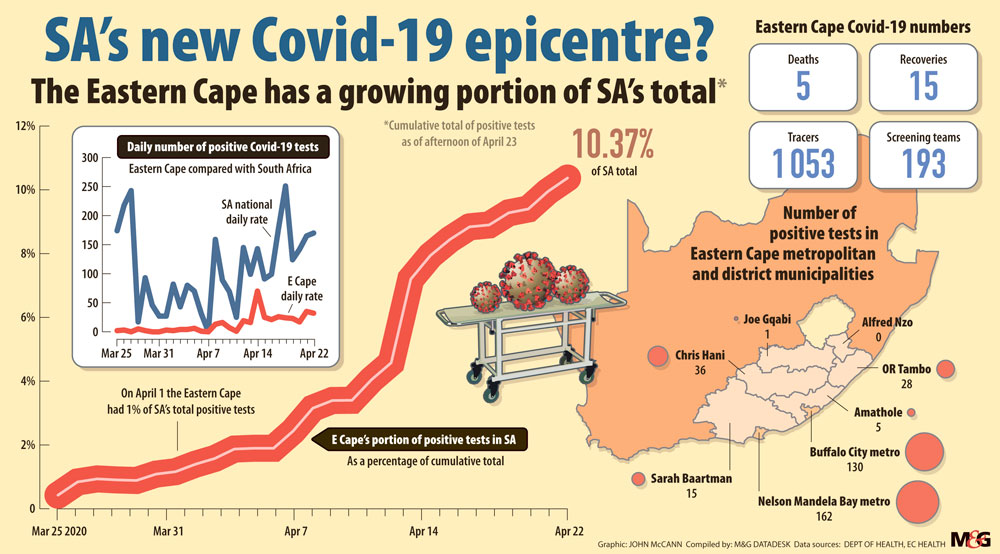
Cases of Covid-19 have surged in the Eastern Cape.
As the number of Covid-19 cases rises rapidly in the Eastern Cape, doctors, nurses and paramedics are battling to do their jobs as frontline responders. In less than a month, the province saw an increase from none to more than 300 cases.
There are complaints across the province, from Nelson Mandela Bay and Cradock to Mthatha, about the shortage of personal protective equipment (PPE), inadequate tracing times and hospitals that don’t have the capacity to handle Covid-19 patients in intensive care.
It has been alleged by numerous emergency workers in the Nelson Mandela Bay, East London and Mthatha areas that the supply of PPE is insufficient, with N95 face masks being scarce or unavailable. Health workers have to resuse gloves and masks when they assist sick people. And there are claims that the D-Germ hand sanitiser has been diluted.
The list continues, but the front line workers the Mail & Guardian spoke to all say the same thing: the Eastern Cape department of health is woefully unprepared for the pandemic and their lives and those of many others are in jeopardy.
Dr Mthembeni Tebelele, whose practice is in KwaDwesi, Nelson Mandela Bay, said the government’s response time in tracing people who have tested positive to Covid-19 needed to improve.
He also said that big gatherings such as funerals and people going to shopping centres were a big factor in the increasing numbers. The Daily Dispatch reported on April 18 that that a third of all cases of Covid-19 in the Nelson Mandela Bay municipality stem from the KwaDwesi funeral of a retired nurse in March, at which there were about 1200 people despite the ban on gatherings of more than 100 people.
“The government needs to provide people with masks just like they are providing free condoms. This is going to kill our people because they are not adhering to any lockdown regulations. We won’t be dealing with positive cases but deaths in this area. Any place where people meet must be sprayed,” said Tebelele.
[td_block_text_with_title tdc_css=”eyJhbGwiOnsic2hhZG93LXNpemUiOiIyIiwic2hhZG93LWNvbG9yIjoiI2Q4ZDhkOCIsInNoYWRvdy1vZmZzZXQtaCI6IjEiLCJiYWNrZ3JvdW5kLWNvbG9yIjoiI2ZmZmZmZiIsImNvbnRlbnQtaC1hbGlnbiI6ImNvbnRlbnQtaG9yaXotY2VudGVyIiwiZGlzcGxheSI6IiJ9fQ==” f_post_font_size=”16″ f_post_font_family=”fs_7″ f_post_font_spacing=”0.9″ f_post_font_weight=”400″ block_template_id=”td_block_template_8″ border_color=”#e60000″ f_h4_font_transform=”uppercase” f_h4_font_size=”18″ f_h4_font_weight=”400″ f_h4_font_spacing=”0.8″ f_h4_font_family=”420″ custom_title=”Latest” custom_url=”https://mg.co.za/article/2020-03-13-live-the-mgs-guide-to-the-coronavirus-outbreak-in-south-africa/” onclick=”gtag(‘event’, ‘clickCovidticker’, {‘event_category’: ‘covidBlock’, ‘event_label’: ‘rightCovidticker’});”]



Visit our hub for the latest data
[/td_block_text_with_title]
An emergency medical service paramedic from Mdantsane, who did not want to be named, said: “Kubi, kunzima [it’s hard].”
The paramedic said their biggest problem was the shortage of PPE and how they have to drive around to clinics and hospitals asking for gloves and masks.
“The hospitals have the problem we have, a lack of gloves and masks. This might not be our manager’s fault but it’s definitely that of the government. We cover a very large area here in Mdantsane, including townships and villages. This is the second biggest township in the country yet no one cares about the work we do or the risk we are putting ourselves and families in,” he said.
Another emergency medical service employee said that in Nelson Mandela Bay they are given five pairs of gloves a day, enough to transport two patients a day. “We have to use two pairs of gloves per patient. Just yesterday [Monday] my colleague was called to a house to pick up a patient who had TB. He was then expected to use the same mask and gloves to pick up another patient.”
She added that another crew member had to transport patients to Livingstone Hospital in Nelson Mandela Bay and used up the masks and gloves he was handed that day. “We are putting our lives at risk yet we have very little to protect ourselves. This is not right and we are endangering others too.”
On Tuesday, as the Eastern Cape’s numbers rose to about 10% of the national infection tally, Health Minister Zwelini Mkhize visited the province and said the national department needed to urgently send more medical specialists, including epidemiologists, analysts and field consultants, to reinforce the provincial team.
According to reports in the Daily Dispatch and The Herald, an angry Mkhize expressed concern that the numbers of Covid-19 cases did not add up. He reportedly sent his deputy director general, Litha Matiwane, to take charge of tracing, screening and testing teams in the city.
The newspapers reported that the minister was presented with a bleak picture by Dr John Black, who heads the infectious disease and HIV unit at Livingstone Hospital.
“We have also deployed senior officials from the national department of health to do a proper audit of the available personal protective equipment and other requirements. This is to ensure the safety and adequate protection of our health workers who are at the forefront. We reiterate that no health worker should be exposed to the risk of infection,” Mkhize said.
Provincial health spokesperson Sizwe Kupelo said the national director will visit hospitals to do an audit of personal protective equipment.
But this is little consolation to the hundreds of people who think the resources might not trickle down to them. The provincial secretary of the Democratic Nursing Organisation of South Africa, Khaya Sodidi, said they told their members a week ago to stop working if there is no PPE.
“Our main concern aside from the safety is that the department is not equal to the task of dealing with this pandemic. For instance, people are showing up at clinics and hospitals that are not ready to deal with Covid-19. The minister was here and he was not taken to Frere Hospital in East London because the wing that is meant to deal with patients is still under construction,” he said.
 (John McCann/M&G)
(John McCann/M&G)
Sodidi added that the union was receiving an inordinate number of complaints from its members.
“How the department is handling this whole thing is clumsy and shows that there was no plan. The increase in numbers is alarming and we will be seeing more,” he said.
Tebelele, who is among the private doctors assisting the government with testing, warned that KwaDwesi was fast becoming a hotspot for the coronavirus in the Nelson Mandela Bay municipality.
“My practice alone has had about 40 people — three positive results just today [Wednesday] only. I notify officials for quarantine purposes,” he said. “The shopping centre here is always full.”
Tebelele added: “How long will it take for the government to act with urgency? They started tracing people who had been at a funeral after a long time, long after the 14 days.
“People are not adhering to instructions. People see quarantine as punishment. This area is a hotspot and endemic area. KwaDwesi should be locked down completely and everyone tested.”
“The government needs to provide people with masks just like they are providing free condoms”