Challenges: Women have trouble accessing care for their newborns as well as facing problems such as poverty, food insecurity and a lack of transport. Photo: File
Pregnant women in South Africa face significant barriers to getting care for themselves and their newborns, prompting renewed calls for grassroots interventions to reduce neonatal and perinatal deaths.
“The persistently high burden of neonatal and perinatal mortality in South Africa reflects deeper systematic challenges,” said Shakti Pillay, a neonatologist at Groote Schuur Hospital in Cape Town.
Those difficulties include inequitable access to quality maternal and newborn baby care; staff shortages; resource constraints and the broader social determinants of health, such as poverty, food insecurity and a lack of transport.
Although the number of live births increased annually in 88% of districts from 2019 to 2020, the longer-term trend shows a national decline in live birth rates.
“There has been a trend of declining live birth rates year on year across most districts with only one district reporting an increased number of live births in 2023-24 compared to 2022-23,” according to the 2023–24 District Health Barometer Report.
“The overall downward trend in birth rates is confirmed by decreasing home affairs [department] birth registration rates.”
The report also found that the projected census estimate of the number of children under the age of one, as used in the District Health Information System, “is in line with this trend” — showing a decline from 1 139 380 in 2021-22 to 1 135 771 in 2022-23 and to 1 132 896 in 2023-24.
Despite declining birth rates, neonatal mortality has remained constant over the past decade. Though it is still within the UN’s sustainable development goals of 12 deaths per 1 000 live births, the goal is to reduce this to below 12 by 2030.
South Africa is likely to achieve this goal in the next five years, but access to well-resourced healthcare facilities needs to be prioritised, and intervention at community level would also reduce the number of newborn deaths, said Sthe Velaphi, a neonatologist and head of paediatrics and child health at Johannesburg’s Chris Hani Baragwanath Academic Hospital.
“Attendance at an antenatal clinic is important. When attending an antenatal clinic, pregnant women get checked for infections like syphilis, HIV and other health issues.
“If you pick them up in time, and we start the motherhood treatment, you might reduce them getting to pre-term labour and also having their babies die from other conditions.
“So, that is the point that they come to the clinic, get managed, get seen, history is taken, pick up those at risk, get managed, and follow them up very closely. That is another level of preventing this.
“Once they are in labour, we need to make sure that they have easy access to the healthcare facilities, so things like ambulances, emergency medical services must be available at all levels, both from the community to the hospital or between the hospitals that you might want to refer a patient to a specialised facility.
“That’s another area where prevention can take place.”
 (Graphic: John McCann/M&G)
(Graphic: John McCann/M&G)
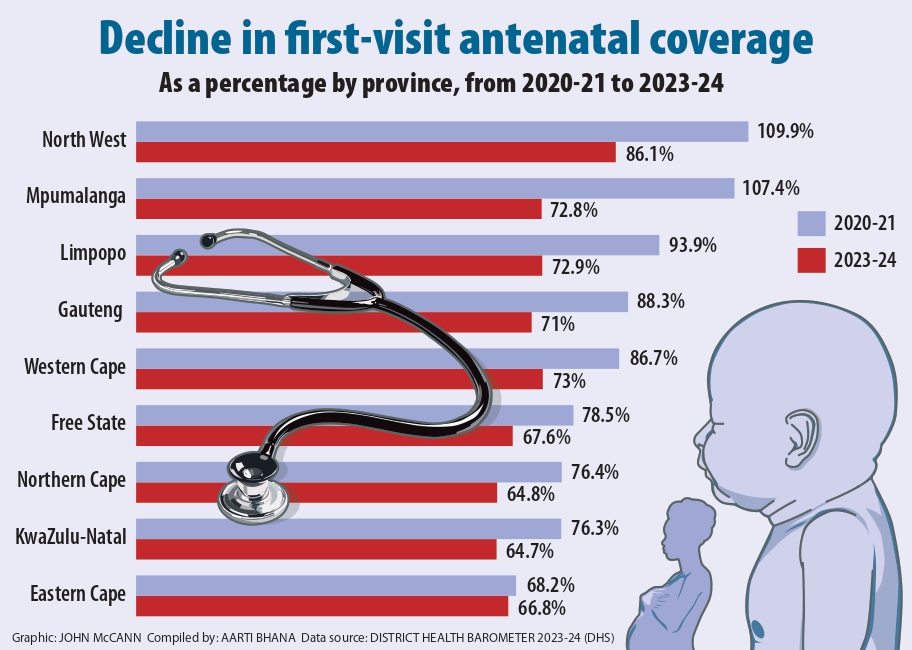
At national level, the antenatal first-visit coverage was 69.4% in 2023-24, down 7% from the previous year’s coverage of 76.4%, and continues a downward trend in antenatal attendance since 2020-21. This was also the lowest documented coverage in the past five years, according to the 2023-24 District Health Barometer Report.
Antenatal first-visit coverage refers to the proportion of patients going for at least one (booked) antenatal visit.
The report attributed this decline to budget constraints in more recent years that might have negatively affected the accessibility of services.
It showed that the number of women who booked for antenatal care in 2023-24 declined to 906 788 from 998 043 in the previous year. Coverage was lowest in KwaZulu-Natal (64.7%) and highest in the Northern Cape (86.1%).
Five provinces achieved a coverage level greater than the national average of 69.4%, while the Free State, Eastern Cape, North West and KwaZulu-Natal were below average.
Over the past two years, 40 districts showed consecutive declines in antenatal first-visit coverage and only Namakwa, Northern Cape, reported a consecutive increase in coverage.
Pillay said neonatal mortalities — deaths during the first month of a baby’s life — were often not a result of inadequate knowledge or technology but “inconsistent implementation of simple, evidence-based interventions, such as antenatal corticosteroids, thermal protection, infection prevention and timely, effective neonatal resuscitation”.
“Ensuring that these essential interventions are delivered consistently and equitably across all levels of care remains one of our greatest challenges — and one of our greatest opportunities to prevent avoidable deaths.”
Last month, Health Minister Aaron Motsoaledi announced that 1 200 doctors would be recruited, as well as an additional 200 nurses and 250 healthcare professionals, to address shortages in the sector.
He also said the National Health Council had decided to purchase 25 000 beds, 80 000 mattresses, 7 655 bassinets for new babies and as well as linen, including sheets and pillows, at a total cost of R1.346 billion.
“It is for that reason that we wish to announce that we have checked province by province what that need [is] in the form of hospital beds and bassinets for newborn babies.
“We remember with a sense of shame how babies were put in cardboard boxes in Mahikeng hospital in the North West province,” he said.
While the announcement to increase resources in healthcare facilities is encouraging, healthcare practitioners said more efforts were needed to ensure that they were properly implemented and could improve health outcomes for newborn babies.
“Increasing posts or procuring equipment, in isolation, will not translate into improved outcomes unless these efforts are embedded within a broader framework of health-system strengthening,” Pillay said.
This included equitable recruitment and deployment; structured onboarding; ongoing clinical training; mentorship; reliable supply chains and strong facility-level leadership, she said.