Postpartum psychosis
I have a story to tell you, but I’m afraid I’m a less than perfect narrator because there are crevasses in my mind that I fall through whenever I try to tell it.
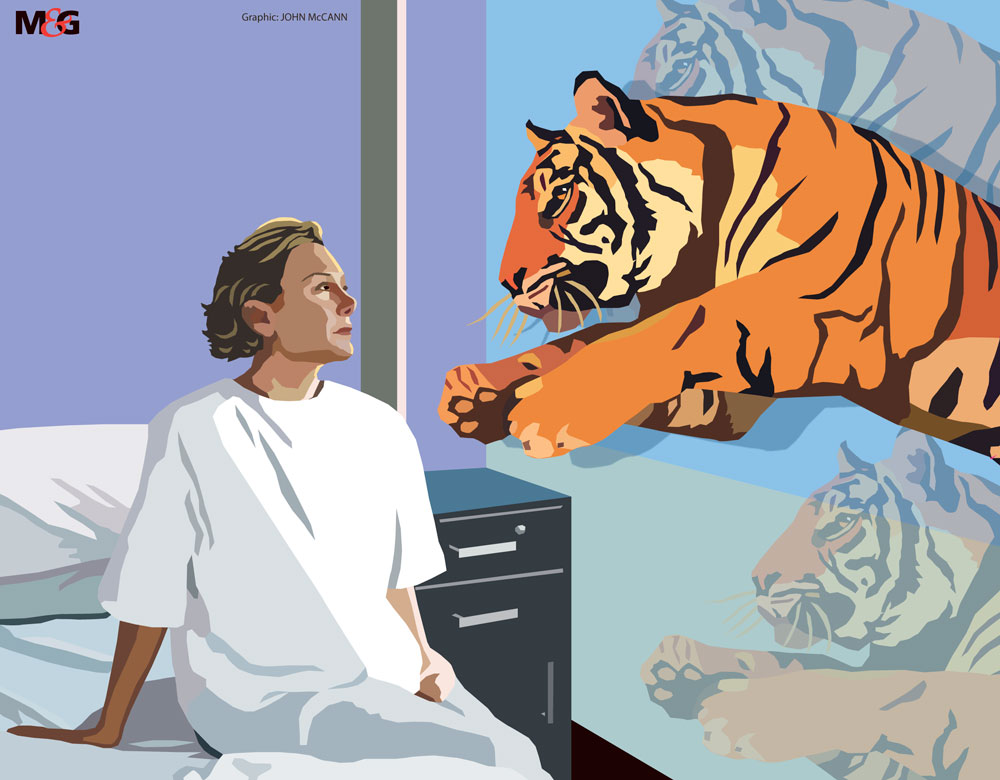
I can pin my finger firmly on the moment I began to wonder whether something was really wrong. From behind me, I heard a child’s voice, small but determined. I contorted this way and that in search of its pestering, persistent owner, but I was alone. This was new. Later that evening, I watched a psychedelic display of electric lions, roaring tigers and the cast of the film Jumanji cavort on the bare blue wall. I wasn’t afraid, just captivated.
Yet a voice, this time my own, questioned how I could be seeing such a spectacle and suggested, gently, that perhaps those around me were right — things were very wrong.
Given that all of this was happening in my room in a psychiatric ward, I was a little late to the realisation party. There had been other not-so-subtle hints – in my belief that my baby had been swapped at birth, for instance, and that road signs were tailored messages for me.
I held these truths to be self-evident and never considered them to be odd, let alone symptoms of an illness.
Yet that’s precisely what they were – evidence of a sick and struggling brain. I was diagnosed with postpartum psychosis, a severe mental illness that affects about one or two in every 1000 women soon after childbirth. It can cause a litany of symptoms, from anxiety and profound sadness to chattiness and euphoria.
Women with postpartum psychosis can rapidly cycle between moods and may experience hallucinations and delusions. Although it’s more common in women who have bipolar disorder, it can affect women who’ve never had mental health issues. It’s a psychiatric emergency that requires urgent treatment because the symptoms can start suddenly and get worse quickly.
At its most severe, it poses a risk of suicide. It can even lead to accidental harm to the baby or infanticide, though this is exceedingly rare.
Unfortunately, infanticide grabs headlines and so women who suffer postpartum psychosis often worry about the stigma of the disease.
Many don’t seek help. One Australian study found that, of those women who had symptoms of postpartum depression, 41% had not sought help within nine months of giving birth. Often, women said they believed their symptoms were normal and would go away.
I can identify. I feel the fear of stigma keenly as I write this, afraid of how you’ll judge me as a mother and as a person. And for months, I too thought my symptoms were a normal part of motherhood and would resolve themselves. This was made easier to believe because the symptoms of postpartum psychosis can wax and wane.
Yet at the peak of my disease a nurse told me I was one of the sickest women she’d seen enter the ward. This shocked me. Sure, I was a bit anxious, a bit bothered, but surely not seriously ill.
Being a parent is meant to be hard, isn’t it? Yes, but it shouldn’t involve thinking trees are angry with you.
It seems obvious now, but thanks to the disease I lacked what’s called “insight” in psychiatric parlance – awareness of how ill I was. Now I know how serious an illness I had and how lucky I was to eventually get specialist medical help.
One in five mothers suffers from depression, anxiety or psychosis during pregnancy or the first year after giving birth, according to a 2016 report by the independent Mental Health Taskforce for Britain’s National Health Service. Many people who tell their stories of severe mental illness do so from a safe distance of years. My story is only months old.
It was my first pregnancy and it had gone well, but as the end was in sight, it emerged that my baby was destined to be a contrary madam. Beatrix was eventually born by emergency Caesarean section in January 2016. Now, as I reflect on the gap between my expectations of bringing her into the world and the reality of it, I see a dark, vast cavern.
I had expected to be the first person to hold her. I’d imagined a celebratory moment as the three of us were together as a family for the first time. In fact, because of the cocktail of drugs I had been given, I spent most of my C-section trying to throw up. My husband was therefore the first to hold her, and clutched her in one arm and a sick bowl for me in the other.
I also bled quite a lot, and when the operation was over I began to shake violently, so I still couldn’t hold her. We returned to the maternity ward, where a nurse tried to get Beatrix to breastfeed, but I was still shaking too much. Ever resourceful, she hand-milked me and collected the milk.
And that’s not the least dignified experience I’ve had since joining the ranks of motherhood.
In those days, I developed beliefs that I now see as the first daggers of disease stabbing my mind. I thought all the nurses were talking about me and had an ever-growing suspicion that my baby had been swapped.
Once back home, I felt anxious and thought that ninja social workers were watching me and plotting to take my baby.
I had to prove to the world that I was a model mum so the spying social workers wouldn’t see any signs of weakness. I therefore hid my suspicious thoughts and fears from everyone.
Even my husband, who has been my best friend and confidant for more than 13 years, wasn’t aware of just how ill I was.
Without the help I needed, over the following weeks I became manic. Five months after my baby was born, things had reached the point where I was terrified of leaving the house for fear of murderous social workers.
Eventually, with the intervention of a community health worker who picked up that something was amiss, I was admitted voluntarily to the mother and baby psychiatric unit (MBU) at St John’s Hospital in Livingston, Scotland. My husband and a nurse had to physically shepherd me to the ward, coaxing me with promises that my baby girl and I could leave again soon. That was an optimistic assessment.
It was a week before I could leave the room, my paranoid mind conjuring up a million ways harm would befall me in the wide-open savannah of the ward. This was to change asthe antipsychotic medication helped to heal my brain, and over weeks I came to see the MBU as a place of safety.
It offered baby massage sessions, weaning classes and splash play activities, all of which enabled me to be the mother I wanted to be.
In short, it was a place that helped me to regrow the confidence that my disease had damaged, making me feel positive about our ability to thrive together at home.
It makes sense that holistic care that nurtures the mother-baby relationship is beneficial for a mother’s mental health. As the United Kingdom’s National Institute for Health and Care Excellence advises: “Women who need inpatient care for a mental health problem within 12 months of childbirth should normally be admitted to a specialist mother and baby unit, unless there are specific reasons for not doing so.”
Yet MBUs are expensive to staff and there is a dearth of published evidence comparing the recovery of patients in them with those in general adult psychiatric wards, where mothers are separated from their babies.
This lack of evidence probably does little to encourage the people in charge of the purse strings to fund MBUs.
There are currently just 125 MBU beds in the UK, and some regions have none at all. The entire United States had zero MBU beds until 2011, when the University of North Carolina at Chapel Hill opened its Perinatal Mood Disorders Inpatient Unit with five beds.
Hannah Bissett is well placed to compare the experience of an MBU with that of a general adult psychiatric ward. In September 2009, she gave birth to her first baby and, two weeks later, was in an adult psychiatric ward with postpartum psychosis. Hannah spent three-and-a-half months in hospitals,initially in two general adult psychiatric wards and then in a small MBU.
She acknowledges that the wards kept her safe. But the separation from her baby was “awful”.
She speaks of the MBU with a smile in her voice: “It was my little haven to be with my baby and for my husband to come in and spend family time together.”
Treatment remains a case of trial and error
Like most women with postpartum psychosis, I was offered medication to treat it, but this can be a bit of trial and error to find the right drug. This may include antipsychotic drugs, anti-anxiety medication, mood stabilisers and antidepressants.
Sally went through six medications and found none that really tackled her disease, leaving her with psychotic symptoms eight months after her daughter Ella’s birth. Her husband scoured the literature to find an evidence-based alternative.
What he found was a game-changer for Sally: electroconvulsive therapy (ECT).
ECT involves passing an electric current through the brain to induce a seizure. When ECT was first used,the seizure would cause painful muscle spasms that could even break the patient’s bones. Today, a general anaesthetic and a muscle relaxant are given, which results in at most a slight twitch of the foot or a tensing of the jaw.
A course of ECT usually involves multiple treatments and its use is controversial, and typically reserved for the most severe of cases that haven’t responded to medication.
Like most treatments, it has potential side-effects and, in the hours following treatment, people can complain of headaches and muscle aches, with a smaller number left tearful or frightened. In the longer term, loss of memory can be a significant issue and this is the source of a lot of the controversy surrounding ECT.
The UK’s Royal College of Psychiatrists sums up the available evidence: “Surveys conducted by doctors and clinical staff usually find a low level of severe side-effects, maybe around one in 10. Patient-led surveys have found much more, maybe in half of those having ECT.
Some surveys conducted by those strongly against ECT say there are severe side-effects in everyone.”
Both Sally and Hannah have memory loss from the period of treatment, which could be attributed to ECT (although it’s hard to separate this from the potential memory impact of the illness itself).
Other people who have had ECT feel very diff erently, saying the treatment has had a permanent, negative effect on their memory. Some go further and say ECT changed their personality or caused them to lose skills, but this remains an area of controversy.
‘Recovery really begins when you walk out of the hospital doors’
As my time in the MBU progressed and I became well, my fearful thoughts were replaced with a lot of questions, such as: What had happened to my brain? I turned to Jessica Heron, a senior research fellow in perinatal psychiatry at the University of Birmingham and director of Action on Postpartum Psychosis, a charity that provides support and information for those affected.
I asked her what we know about the risk factors for postpartum psychosis. “Very little, really,” she said. “The best guess at the moment is that biological and hormonal factors are involved. There have been some studies into the most likely candidates and they haven’t found anything consistent. We do know it runs in families more often than you’d expect. We know there’s a strong link with bipolar disorder. So some of the risk factors that have been found in bipolar, like sleep disruption, [maybe implicated].”
Unfortunately, into the neurobiology of both bipolar and postpartum psychosis, there are many theories – genes have been implicated and chemicals that have been incriminated – but no clear answers.
I asked Heron why so little of the biology of postpartum psychosis has been elucidated. “Because it’s been perceived as rare, I think funders haven’t seen it as a priority,” she replied. The knowledge drought around my illness left me feeling that science, my usually faithful mistress, had failed me.
Thankfully, a new friend came to my rescue and provided the insight and understanding I sought: storytelling. Recording my story was therapeutic.This started in the hospital, initially through the medium of photos because I couldn’t focus or stay still long enough to write anything.
Despite the rich medium of imagery, I was pleased when I could once again communicate using the written word. Like taking photos, writing was therapeutic and formed a key part of the healing process for me. I wasn’t alone. A 2006 review of 146 randomised controlled trials of written or spoken “experimental disclosure” (disclosing information, thoughts and feelings about personal and meaningful topics) found significant positive effects across a range of measures, including psychological health and physiological functioning.
The following year, Matthew Kreuter and his colleagues devised a hypothesis about why narrative communication, such as storytelling, journalism and testimonials, might benefit cancer patients. They suggest narrative writing allows you to impose order on the chaos that disease foists on your life.
I think this applies to mental illness too and gets to the heart of why, for me, storytelling has been integral to my recovery from postpartum psychosis. I had felt like I was standing in a hurricane of these terrifying thoughts, and writing was like stepping into the quiet eye of the storm where I could physically pin my thoughts on to the page and stop them constantly whizzing around my brain.
For someone used to being in control, this was a godsend. With the combined therapies of medication, the MBU and storytelling, I became well enough to go home after six weeks. Unfortunately, the road to recovery from postpartum psychosis is often beset with challenges.
About three months after being discharged, I developed postpartum depression, an experience Heron reassured me is more common than not after postpartum psychosis, and I was hospitalised in the MBU for a further three months. It wasn’t until I spoke to Hannah that I realised recovery really begins when you walk out of the hospital doors.
She says: “I describe it as being shattered into a million pieces and then rebuilding it all gradually the main thing being [having] the confidence in my own abilities.”
Writing this article is part of the process of rebuilding my confidence. Being adept at writing is core to my identity. As well as understanding and processing what has happened to me, I needed to do this to prove post-psychosis me could still write.
Women who have experienced postpartum psychosis have more than a 50% chance of another episode following a subsequent birth.
It’s a bridge that my husband and I will cross in the future. For now, I’m focused on the present and grateful that the MBU and various forms of storytelling have helped me to move from a place of acute illness to being at home and well with my baby girl.
This article first appeared on Mosaic and is republished here under a Creative Commons licence.
