Malegapuru William Makgoba's scathing investigation helped blow the lid of the Life Esidimeni tragedy. Read what it taught him. (Delwyn Verasamy, Mail & Guardian)
COMMENT
In September 2016, Health Minister Aaron Motsoaledi asked me to investigate the deaths of, at that time, 36 mental health patients as part of the Life Esidimeni tragedy. The deaths came after the Gauteng health department removed about 1 700 long-term psychiatric patients from state-sponsored care at Life Esidimeni facilities in 2016 and placed them into the custody of mostly unlicensed nongovernmental organisations.
Since I released my 2017 report, the number of people who died as part of what became known as the Gauteng Mental Health Marathon Project has gone up four times and now stands at 144.
People have asked me what I learned from the Life Esidimeni saga. I learned many things but three, in particular, stand out for me. They tell us how our history informs our present and what we need to fix to change our future.
My first lesson was that democracy might have dawned for South Africa, but we can’t say the same for bioethics — or the tenets that guide the way we practise medicine and care for our people. In fact, some of the central ethics that govern our health professionals have not been reviewed for 50 years. We continue to live under what I call “colonial and apartheid” bioethics that allow for the kind of political co-option that we saw in police cells under apartheid and in the halls of the Gauteng health department with Life Esidimeni.
I’ll start with a short story. There is a classic book in medicine, entitled A Sick African: A Clinical Study, written by a South African-trained doctor, Michael Gelfand, in 1948. The book describes two types of African patients: The so-called “sophisticated” and the “non-sophisticated”.
The “sophisticated African” patient has apparently begun to adopt the habits of Western civilisation, unlike his allegedly unsophisticated peer, which Gelfand describes:
“Their villages are badly planned and are often situated in malarial or tsetsefly areas. They know nothing of the importance of taking precautions against disease. They have no idea of cleanliness, and their huts are breeding-grounds for parasites and germs of every kind. Of sanitary arrangements, they know nothing at all.”
This text was written 70 years ago and came to be regarded as a classic — that tells you what foundations it laid for ethics in Southern Africa.
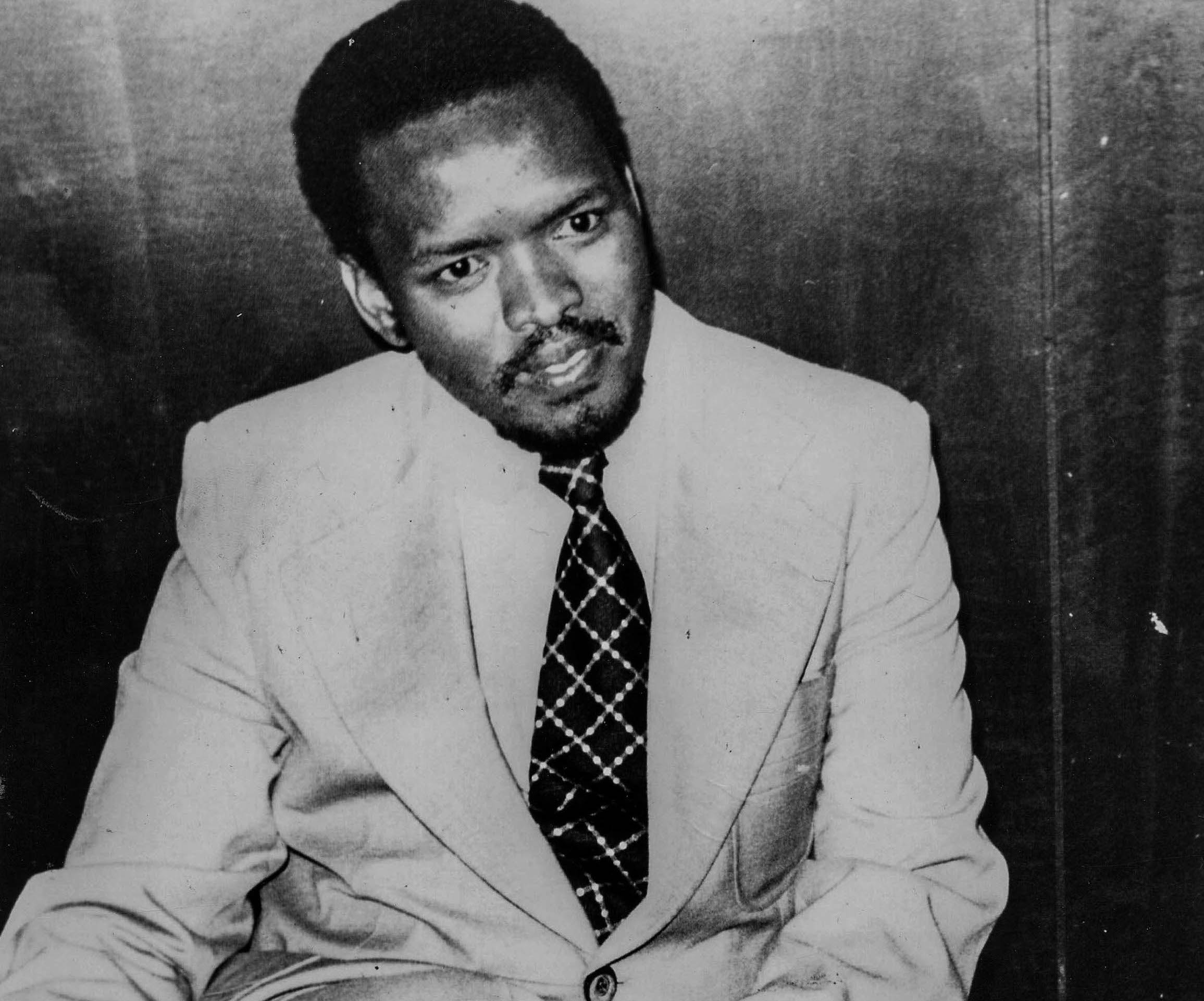
Activist Steve Biko was examined by a doctor shortly before his death. The clinician denied Biko medical care following torture at the hands of police. (Daily Dispatch)
Let’s come to South Africa and the death of anti-apartheid activist Steve Biko. It happened in a South Africa in which doctors were absolved of having to take “political decisions” and were allowed to claim that Biko’s death at the hands of police while in detention was owed to natural causes. In so doing, doctors were backed by the then South African Medical and Dental Council, which would eventually form part of today’s Health Professions Council of South Africa (HPCSA).
It was only eight years after Biko’s death that one of the doctors who examined him and denied him medical treatment was struck off the medical roll.
That is apartheid bioethics. So too was the government’s “aversion therapy” programme headed up by psychiatrist Aubrey Levin, a teacher of mine at what was formerly the University of Natal. Levin administered shock therapy to men who had sex with men under the guise of supposedly “curing” them of their sexual orientation, flouting all ethical principles.
Levin is now a recently paroled sex offender living in Canada, the Canadian Broadcast Corporation reports.
When we got our independence in 1994, we did not sit down and ask ourselves what kind of ethics we need in this new country with a new human rights-based Constitution.
In the Life Esidimeni exercise, this has been exacerbated.
My second lesson was about denial. In our country, we go into denial when we are confronted with the truth. Denial is, in fact, a very important part of our political make-up.
In the 10 years of Aids denialism that took place under former president Thabo Mbeki and the late health minister Manto Tshabalala, 330 000 people lost their lives, according to 2008 Harvard University estimates published in the Journal of Acquired Immune Deficiency.
Doctors were intimidated into not signing death certificates that listed HIV as the cause of death because Mbeki and Tshabalala continued to question the causal link between HIV and Aids.
South Africa has a long history in which science was abused to promote or underpin political decisions. We saw something similar in the Life Esidimeni investigations when some of the death certificates were not even signed by doctors but by lay people.

When employees questioned about her decision to move almost 1 700 mental health patients from Life Esidimeni care, former MEC Qedani Mahlangu allegedly asked staff, “Do you work for us or Life Esidimeni?”
My third lesson was that, if you put a “sombre thought” forward to politicians, you run the risk of being called a “counter-revolutionary”. Anyone who disagrees with the ruling authority becomes “an enemy of the state”.
Politics still prevail over and shape the practice of healthcare in South Africa.
You hear talk about fraud within the health sector, about the Special Investigating Unit looking at leading politicians. But I have yet to find anyone who has actually been arrested and locked up in jail. South Africans want to see someone wearing orange, serving time for what they have done and we have not seen that.
Someone steals money, and we find a way of forgiving them. In fact, when I was looking at Life Esidimeni, that’s one thing that came across in my interviews with officials: this sense that we were somehow making examples of them while others were being forgiven.
In the past 24 years, bad political decisions have cost our country dearly with health scandals — morally, ethically and economically.
South Africa must begin to redefine ethics within healthcare in a way that is in line with our Constitution but also the creation of our new society. In a changing, transforming society we cannot afford to rely on ethical crutches — including guidelines from the HPCSA that regulate most professionals — that have scarcely been reviewed for the last 50 years.
Malegapuru William Makgoba is the health ombud at the Office for Health Standards Compliance.