Helping hand: Hauwa Ojeifo owns an organisation that helps to support women facing mental health issues.
A circle of bright red and green plastic chairs and a pull-up banner are the only signs that a meeting is planned in the schoolhouse in Ikeja, the capital city of Lagos State in Nigeria.
It is a Sunday evening. Two small fans puff hot air into the small classroom with its fraying brown carpet and window overlooking the street. The sound of voices from outside drifts in through the door. The first woman to arrive is dressed in a flowing dress crafted in brightly coloured Ankara fabric. Then others start trickling in. Soon the room is packed and “Safeplace”, Nigeria’s first support group for women with mental health issues, gets under way.
The facilitator is a petite 26-year-old. Dressed in a purple hijab and black cardigan, Hauwa Ojeifo reaches out to a young woman with closely cropped hair. At first, she struggles to speak; her body wracked with deep sobs, but then her story comes tumbling out. She tells of the debilitating mood swings that have “changed her personality”.
Ojeifo is so adept at her role — prodding, supporting, encouraging — that you could be forgiven for thinking she was a trained psychologist rather than the investment banker she is by profession.
The support group is her brainchild and the result of her own journey with mental illness and depression. Two years ago Ojeifo was diagnosed with bipolar disorder and posttraumatic stress disorder (PTSD), prompting a desire to help others grappling with similar issues.
Watch: Your period could be messing with your mental health
Bipolar disorder is a mental health condition marked by extreme mood swings that alternate between emotional highs — or mania — and depression, United States research body the Mayo Clinic explains. Triggered by experiencing trauma, PTSD’s symptoms include flashbacks, nightmares and anxiety and can appear immediately or after years.
But in Nigeria, mental health support from trained professionals is almost impossible to access. A 2018 census by the Association of Psychiatrists in Nigeria found there are only 250 psychiatrists in a nation of close to 200-million people . The few practitioners in private practice charge fees that are out of the reach of most.
Ojeifo’s own struggle with mental illness began in about 2012 when she started experiencing severe depression while studying for a master’s degree at the University of Reading in the United Kingdom. She was raised in a high-achieving family with very strict parents. The pressure to excel was enormous, she says. “I couldn’t just pass; I had to be the best.”
The strain finally took its toll. “My hair was falling out. I had fainting spells, waking up on the floor and realising four hours had passed.” When a doctor who suspected she was battling depression advised her to take a year off to regain her mental equilibrium, she didn’t know how to tell her parents. “What was I going to say? I want a year off because I have a headache?” She finished her degree, but when she returned to Nigeria to take up a job in banking, things got worse.
She was sexually harassed, Ojeifo says. Coupled with her depression, things proved quite overwhelming to handle. But she couldn’t afford regular professional help.
In Nigeria, about 4% of the national budget is allocated for the health of almost 200-million people, 2018 budget data shows. In 2006, a World Health Organisation report noted that there were only eight federally funded psychiatric hospitals available to a population of over 140-million in 2005. Twelve years later that has not changed. A 2013 National Mental Health policy, promising mental health care at the primary care level, has never been implemented. The number of trained psychiatrists also continues to drop as many specialists leave the country in search of better working conditions abroad.
To process her trauma, Ojeifo started writing about it on her blog. “In Nigeria, victims of sexual abuse are often shamed,” she says. “At first I wrote bits of my experience on my blog and social media in the third person so nobody would suspect I was talking about myself.”
But her underlying mental illness started to manifest more aggressively. “I began to break bit by bit,” she remembers. “The highs were getting higher and the lows were getting lower. I was starting to have suicidal thoughts.”
One Sunday afternoon in 2016, she experienced an “urge” to end her pain. “It was like a rush: I just knew I needed to end my life.”
A cousin who had been diagnosed with PTSD came to her rescue and introduced her to Project Alert Violence Against Women, a nongovernmental organisation that promotes and protects the rights of women and girls. It was a turning point for Ojeifo. “Finally, I didn’t need to hold back anymore and I could start talking about the problematic things that I had suffered from.”
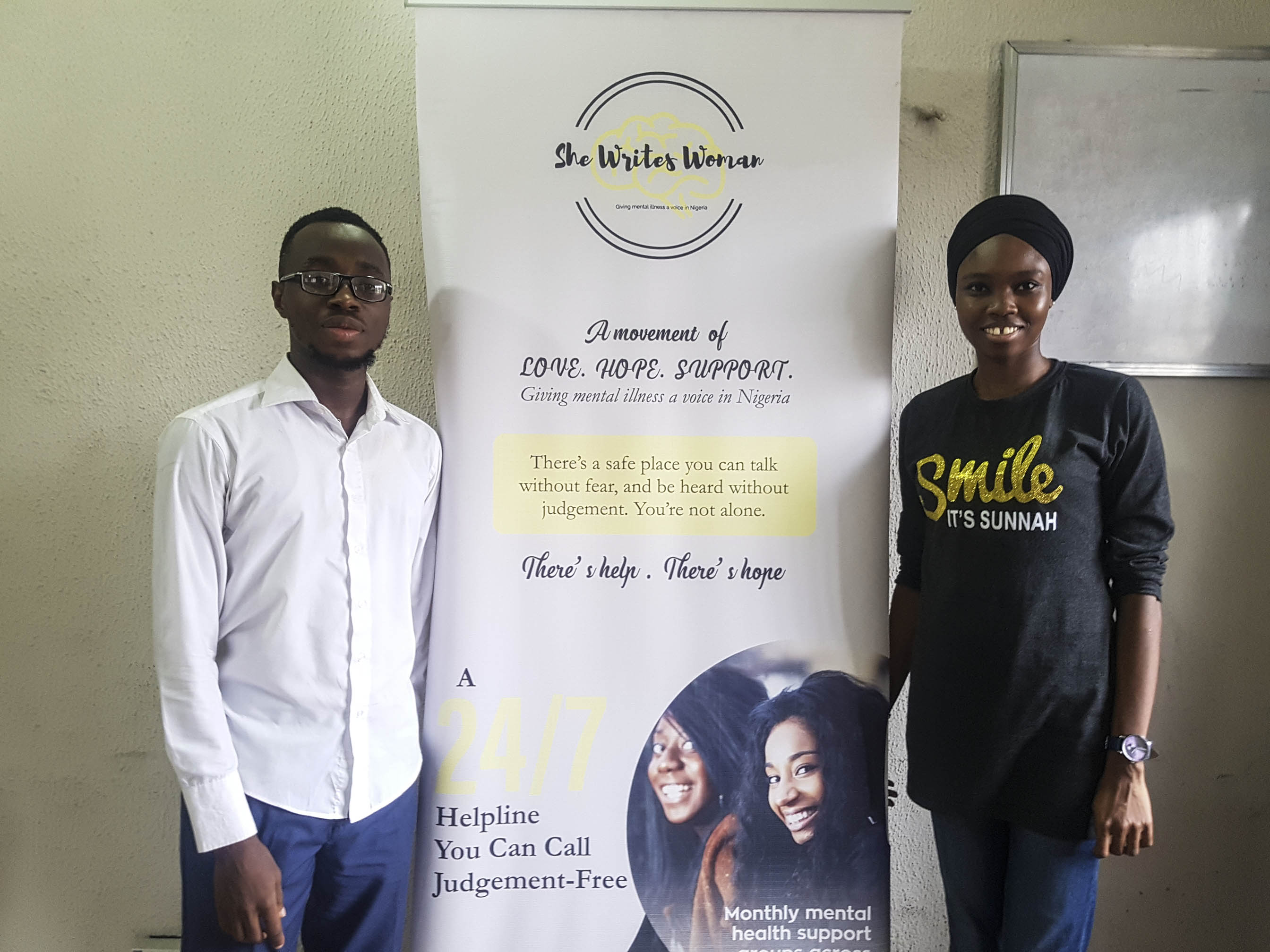
SheWritesWoman has grown to include a helpline and also has more than 20 volunteers, including Olamipo Adeniji and Shakirat Bashir, as well as a psychiatrist. (Shola Lawal)
It was during this dark time that her blog, SheWritesWoman, transformed into something with a purpose beyond her own pain. She had run out of money to pay for psychologists and was desperate to connect with people who “got” what she was dealing with.
SheWritesWoman became her refuge and her therapy. “I was tired of people telling me depression was just a phase, or that I should pray to God for help.” She quit her job and decided to build SheWritesWoman into an organisation that would help people with mental illness.
Opening up to people online about her trauma and giving wellness tips was initially a way for her to deal with her struggles. Then thousands of women started signing up to follow her inspiring messages and selfcare tips for dealing with depression, anxiety and other mental disorders, and the blog turned into an online counselling platform.
“Many people need to talk to someone, and need someone who knows how to talk to them,” she says about her decision to take her counselling services one step further. “I had this telephone line that I wasn’t using, so I decided to start a helpline. There was nothing like it in Nigeria at the time.
“From having been on the other side, I know the worst hours are at night when everyone has gone to bed and you take off your fake smile and your makeup.”
Ojeifo’s helpline hasn’t stopped ringing, and her organisation now has over 20 volunteers — including a registered psychiatrist.
Most callers are between 25 and 34, but some are as young as 15. Although SheWritesWoman is an organisation for women, men now make up 18% of those contacting her helpline, and Ojeifo says another trend is that 18- to 21-year-olds are starting to reach out more. “The student population is often wrongly ignored,” she says.
“Exam pressure, romantic relationships and the turbulence that comes with early adulthood are some of the many problems this segment deals with.”
There is no provision for mental health screening for children or adolescents in Nigeria — a topic Ojeifo is especially passionate about. “More youths are turning to substance abuse and there is a very bleak outlook on life,” she says. “About half our population is younger than 30.”
Ojeifo’s interventions have now extended to the Safespace support groups. Over 400 people have registered to attend in Lagos alone, and groups have also been established in four other states, including Abuja, Nigeria’s capital.
This is why platforms like SheWritesWoman are useful, she says. It has the potential to reach people in far-flung and remote areas, and to provide cheap, convenient support — an important factor considering the high levels of poverty in Nigeria. “Many people can’t travel to access mental healthcare and also want confidentiality and anonymity.”
The helpline and support groups cater to an offline, lower-income audience too. Mobile phone penetration in Africa’s largest economy stands at a staggering 84%, according to the 2018 Nigerian Mobile Report by online commerce giant Jumia. But data remains expensive. “The need is great”, Ojeifo says, pointing to the rise in callers who request to chat on WhatsApp, which is cheaper than paying for airtime.
According to Ojeifo, the associated stigma of mental illnesses means many people don’t try to access support at all, even online where they can be anonymous. Many of her clients have confessed that they avoid commenting or “liking” SheWritesWoman’s Instagram posts so that their followers are not alerted to the fact that they might be living with mental illnesses.

250 psychiatrists in a nation of 200-million people. You do the math. (Reuters)
Virtual counselling, sometimes referred to as e-therapy may or may not involve psychologists. It has its supporters and detractors.
Nigerian psychiatrists, most of whom are overburdened by the high patient rate, are supportive of e-therapy. Because it seems to encourage people to reach out, despite the stigma attached to mental health, it is a welcome development, says Temitope Afolabi, a consultant psychiatrist at the Federal Neuro Psychiatrist Hospital in Lagos.
When researchers in the UK connected about 700 new mothers at risk of postpartum depression telephonically to women who have recovered from the illness, new moms halved their risk of developing the condition, a 2009 study published in the British Medical Journal found. In 2014, follow-up research published in the journal Trials found that this kind of peer support was also cost-effective.
But many studies point to a need for more research into how e-therapy stacks up against a traditional psychologist’s couch — including 2016 research published in the Canadian Medical Association Journal. The study, which reviewed more than 1 000 articles on internet-based therapy found only one small, 2008 clinical trial that compared online therapy with face-to-face counselling. It found no difference in how well patients did on in person versus online therapy, researchers argue in the Journal of Anxiety Disorders.
But those who saw a psychologist in person were more likely to have a better understanding of therapy and enjoyed it more.
Tobiloba Ajayi is a lawyer and disability advocate living with cerebral palsy. She is a regular at Safeplace meetings. She says she has bounced back from two suicide attempts and needs the support to avoid relapses. “Support groups like these are important because many people don’t have the luxury of seeing a therapist. People need to talk to people who will hold their hand.” — Additional reporting by Joan van Dyk