Fewer people are getting tested for HIV than last year.
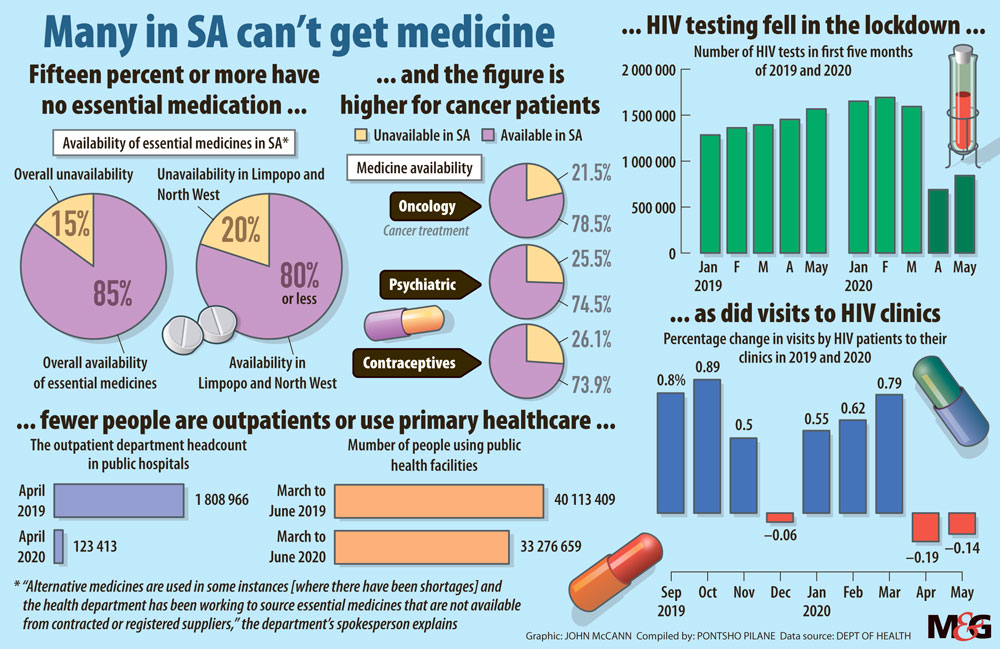
Testing for HIV at public health facilities declined 57% during the first month of lockdown instituted because of the Covid-19 pandemic in South Africa, according to data from the national health department.
About 1.6-million HIV tests were conducted in March. In April that number dipped to just fewer than 690 000 tests, just after the lockdown was instituted at the end of the previous month.
Additionally, more than twice as many people tested for HIV in April last year compared to this year, showing one of the devastating effects the Covid-19 pandemic has had on access to healthcare services.
HIV testing services in public clinics and hospitals were not shut down during lockdown, because these facilities were considered essential services. However, the restrictions of movement resulted in a decrease in HIV testing, because community testing stopped.
“The department introduced innovative testing methods, such as HIV self-testing, in collaboration with partners. The HIV self-test kits were distributed online and at community pharmacies during the lockdown,” said national health department spokesperson Popo Maja.
For instance, people can request that HIV self-testing kits be delivered to them at no cost, through organisations such as Care Works. These free HIV self-tests were also distributed to communities during Covid-19 community screening.
Disruptions to HIV treatment and services could have far-reaching effects.
Early modelling convened by the World Health Organisation (WHO) and UN AIDS estimated that a six-month disruption of antiretroviral (ARV) treatment could lead to more than half a million additional deaths caused by AIDS-related illnesses in sub-Saharan Africa.
This has considerable implications for South Africa’s public health system because about 72% of South Africans say a public clinic, hospital or other public institutions are the first places they go to for health service, according to Statistics South Africa. A little more than a quarter say they would first consult a private doctor, private clinic or hospital if they were to fall ill or have an accident.
Civil-society coalition Stop Stockouts Project (SSP) said there had been stockouts and shortages of essential medicine such as HIV treatment across the country. According to its monitoring, there were 80 stockouts recorded: contraceptives made up a third of these, with paediatric HIV treatment and vaccines at 23% and 16%, respectively.
“We have recorded instances of HIV-treatment shortages, as well as shortages of chronic other medications,” said SSP’s project manager Ruth Dube.
 (John McCann/M&G)
(John McCann/M&G)
In July, the coalition also noticed an increase in stockouts for particular fixed-dose, combination medication HIV treatments in six of the nine provinces. Fixed-dose, first-line HIV drugs were also not available, according to the coalition. These drugs are accepted as the best medicine for someone who is starting treatment.
Additionally, South Africa is in the process of switching adult HIV patients to a more effective drug with fewer side effects.
Maja said that although the health department has faced challenges because of supplier constraints, it has embarked on a weekly allocation of stock to provinces to ensure equity of supply.
The coalition also noted that medications used to treat conditions such as tuberculosis, mental-health illness, and birth control were also not available across the nine provinces over July. “If people are unable to access their medicine through their usual channels they will either suffer financial, psychological and physical stress trying to obtain it through other channels or they will suffer the consequences of being untreated,” Dube said.
“With ARV treatment interruption, the risk is developing drug resistance and losing control of viral suppression. With contraception, the risk is an unplanned pregnancy; with chronic diseases such as mental health conditions, treatment interruption could have far-reaching impacts on individuals and communities.”