The next three to five years will require the continent to ensure there is sustainable business beyond Covid-19.
South Africa needs to drastically improve its data capturing, surveillance and monitoring of immunisation for children under the age of five to prevent outbreaks of measles and whooping cough — against which they are underprotected.
This emerged last week from interviews with some of the country’s top paediatricians, virologists and public health specialists.
They were speaking after the health department said during Global Immunisation Week that its child hexavalent and measles inoculation doses fall below acceptable targets for maximum effect. The hexavalent vaccine protects children against diphtheria, tetanus, pertussis (whooping cough), poliomyelitis, Haemophilus influenza type B and hepatitis B.
Ntombi Mazibuko, a child health consultant to the United Nations Children’s Fund (Unicef), said Covid-19 has impaired coverage that was already below par before the pandemic.
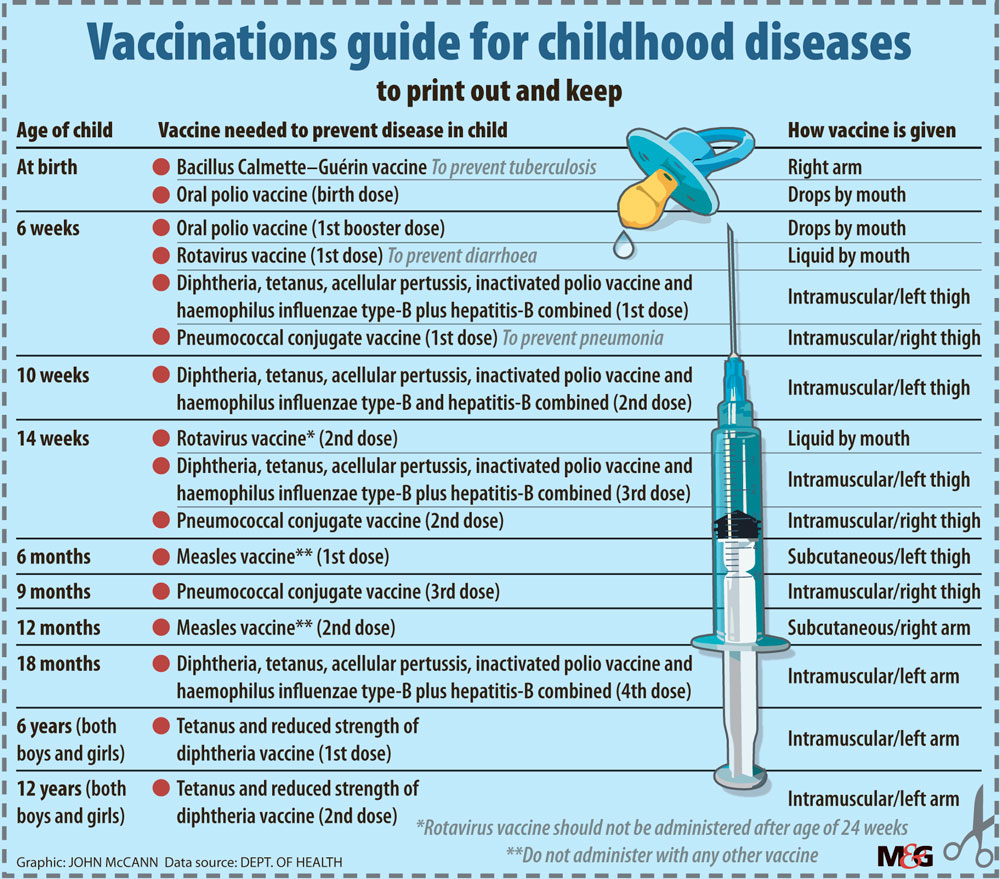
“Our [South Africa’s] childhood immunisation coverage has been suboptimal. We’ve never reached global targets. The World Health Organisation [WHO] coverage target for measles first dose is 90% [given at the age of six months] and the second dose [at 12 to 18 months] is 95%. The hexavalent [six-in-one vaccination, given at six, 10 and 14 weeks, with a booster dose at 18 months) is set by the WHO at 80% coverage. We never got to those levels — and Covid has worsened the picture,” she said.
Mazibuko said few health districts hit these targets, which aim to provide full protection against outbreaks by providing herd immunity.
Mazibuko said some districts were at 70% of hexavalent vaccine coverage — 10% short of the target — and others fell 5% short of the second measles booster dose coverage target of 90%.
“We need to do much more to improve the situation, otherwise we’ll end up with a resurgence of vaccine preventable diseases for children under five,” she warned.
An explanation of how this escalates break-out infection risk, especially the more life-threatening and infectious measles and whooping cough, comes from Professor Brian Eley, head of paediatric infectious diseases at the Red Cross Children’s Hospital in Cape Town.
“The problem with the pertussis vaccine is that you need a full primary dose [consisting of incremental shots at six, 10 and 14 weeks] and a booster secondary jab at 18 months,to give adequate protection. Secondary protection is not sustainable for more than three to six years before kids again become susceptible. If you have below par coverage of pertussis, infants under one year old, more importantly those under six months, are particularly vulnerable to severe pertussis and may end up in ICU with pneumonia complications. The mortality risk in these age groups is particularly high, and the hexavalent vaccine covers this disease as well.”
A systemic weakness in South Africa’s overall childhood vaccination programme is the questionable integrity of data being collected, which means that vaccination figures are probably inaccurate. A clinic may not be able to find a child’s vaccination history because South Africa’s population is highly mobile. This may result in the child not getting crucial doses, which reduces protection — and incorrect data is captured.
Unless the child-minder has the Road to Health record card, vaccination staff may assume earlier doses were given. Children are often brought to clinics by other family members because the mother works in a faraway town or province. Conversely, the child may travel with its mother, who may use a different clinic that is unaware of the child’s vaccination history.
Johann van den Heever, chief of the expanded programme on immunisation until 2016, says his biggest concern is how accurate data is. “The national health department doesn’t mention all the other vaccinations. If things are not okay with these two [measles and hexavalent], what are they not saying about the others?”
The Johnson & Johnson Covid-19 vaccination rollout is underpinned by an electronic vaccination data system, (EVDS), but the childhood immunisation service enjoys no such luxury.
This means that neither the national health office, nor the WHO in Geneva can instantly select and interrogate data on a dashboard. Instead, clinic staff laboriously note down childhood immunisation data, load it on a computer, and then send it to their district office, which in turn collates it and passes it to the province, which transmits it to the national health office. This data then gets sent to Harare, where the WHO’s East and Southern African hub is located, and then on to Geneva.
South Africa’s childhood immunisation data centralisation process takes months, rendering timely monitoring and surveillance virtually useless.
Van den Heever said: “The system is not compatible with reality. If you don’t connect the vaccination the child gets with the age of that child, you have a problem. We have a different system for vaccine procurement and a different system for vaccine management. The two should speak to one another. We need an electronic vaccination register connected to the kids unique ID number at birth, which tracks all vaccinations for the rest of their life.”
Van den Heever campaigned in vain for this before he resigned from the service.
Christine Muhigana, Unicef’s South African representative, said the broad-ranging effect of Covid-19 on the health and wellbeing of children “is laid bare when we look at routine vaccination rates”.
“We need to renew our focus on child health services and promote the use of vaccines to protect children from preventable diseases.”
She echoed Mazibuko, adding: “The drop in routine immunisation coverage among children under five years of age over the past 13 months could lead to a resurgence of vaccine preventable childhood diseases as community vaccination coverage is compromised.”
Eley said his chief concern was that if a sufficiently large pool of infection developed in unvaccinated or under-vaccinated children, it could spread to every province.
As for Covid-19, he said most children were inherently at lower risk of catching it than adults, except for a small sub-set — below 1% — that developed multisystem inflammatory disease, speculatively put down to genetic factors.
Children under 12 months were generally more susceptible to symptomatic Covid, and a small number of these would need to be under intensive care.
Professor Greg Hussey, a member of the ministerial advisory committee on Covid-19 and director of Vaccines for Africa, based at the department of paediatrics and child health at the University of Cape Town, estimates that South Africa’s childhood vaccination coverage has dropped by about 20% since pre-Covid-19 days.
“That’s a concern because children are becoming more vulnerable to vaccine-preventable diseases. It’s like a keg fire in a sense. You just need measles in a preschool — one little spark, to set it off,” he said.
Hussey said Covid-19 had affected all routine health services. “It’s a two-edged sword; while people move around less and are thus less vulnerable to infection, they’re also less inclined to seek out health services.”
He added: “We’re approaching winter and I think the realities and concerns are about pertussis, because it’s a respiratory disease. Next is measles, which tends to spread during late autumn and in winter.”
Mazibuko agreed that the immunisation data were unreliable but saw solutions on the horizon.
“I’m sure the EVDS will be adapted for our children, which would boost things hugely. Also, the national health department is implementing vaccine catch-up drives across provinces. There’s been huge social mobilisation on getting kids to clinics. It’s just that the data system can’t tell us where we are.”
She said Unicef South Africa was providing technical and monitoring support to the vaccine catch-up drive in all 52 health districts.
Problem of poor data on vaccine coverage known 10 years ago
The last major outbreak of a childhood disease in South Africa was in 2009-10, when 18 000 children were confirmed by the Institute of Communicable Diseases as having measles.
One study, at the Red Cross War Memorial Children’s Hospital in Cape Town, between 1 November 2009 and 31 July 2010, showed 1 861 children had been diagnosed with measles, of whom 30% (552) were admitted, 68% had pneumonia and 48% diarrhoea. Their average age was 7.36 months and 73% of them had HIV. Eighteen children died — 3% of all admissions — and 15 (83%) were under a year old, with higher mortality among those with HIV. Of all those admitted, 65% were under nine months old.
The authors of the article, published in the September 2012 edition of the South African Medical Journal, pleaded for the urgent improvement and supplementation of vaccine coverage, especially in under-serviced areas, saying this required, “sufficient political will”.
According to the December 2020 newsletter of the African Society for Paediatric Infectious Diseases, knowing the immunisation coverage before the Covid-19 pandemic would have provided a better understanding of the potential negative consequences of the interruption of immunisation as a result of the pandemic.
Coverage of the third dose of the diphtheria, tetanus, and pertussis (whooping cough) vaccine (DTaP3) was used as an indicator of how well countries were performing in routine immunisation services, the article said.
It added that on 15 July last year, the World Health Organisation (WHO) and the United Nations Children’s Fund (Unicef) reported a decline in the number of children receiving routine vaccines worldwide because of gaps in the delivery and uptake of immunisation services caused by the Covid-19.
“These disruptions further reduce vaccine coverage, which has already been hampered by a decade of stalling coverage,” the authors said.
According to the WHO and Unicef report, this is the first time in 28 years that a substantial drop in the number of children completing three DTaP doses has occurred.