Tholakele Memela sought help when she realised the symptoms for HIV and a sangoma’s calling were similar.
It is a hot day in KwaZulu-Natal and the sun beats down on the dusty roads of a township outside Pietermaritzburg’s Edendale suburb. Leading away from Edendale Hospital, the streets wind up and down the hilly neighbourhood. A lone dog crosses the path and scrapes under the fence of a yard where three graves are lined up in front of a small house.
Down one of the winding roads, Tholakele Memela sits on a reed mat in her consulting room, her legs stretched out in front of her. A guitar balances on a pile of clothing. In the corner is a shelf holding plants and jars of traditional medicine. She lights a candle, which does little to light up the dark room. Then, with her head bowed, she prays out loud.
Memela is a sangoma. Red and white beads adorn her ankles and her wrists, and hang loosely around her neck.
“In the mid- to late-2000s I realised that I needed help because I would take clients in as initiates, thinking that the reason my treatment wasn’t working for them was because they had the calling, only for them to die during initiation,” she recalls.
Memela says the symptoms of HIV and the ancestral calling are similar – something she has experienced first hand. A person infected with HIV and not on treatment can develop symptoms such as weight loss, fever, diarrhoea and a cough, according to the World Health Organisation.
Back in 1983, a younger Memela had suddenly fallen ill. “I had lost a lot of weight and suffered from splitting headaches. Then I developed a persisting cough, but there was no sign of tuberculosis or asthma. Nothing,” she recalls.
“A lot of people with HIV present to us with these symptoms. So, unknowingly, you would just start the rituals for initiation and the person ends up getting sick and dying.”
Where tradition meets modern medicine
http://bhekisisa.org/multimedia/2016-03-02-where-tradition-meets-modern-medicine
HIV and TB training
This is the reason she was one of the first traditional healers to participate in a training programme run by iTeach, an HIV and tuberculosis nongovernmental organisation. It provides basic HIV and tuberculosis training, followed by a month of practical training at local clinics.
“Our graduates are able to screen for TB, test for HIV, record results and prepare patients for treatment,” says iTeach director Krista Dong.
But this marriage between Western and traditional medicine was frowned on by other sangomas in the area. Memela and the other traditional healers who took part in the programme were accused of “agreeing with the whites that the use of indigenous medicine must be stopped, that it doesn’t work”.
“But that was not the case,” says Memela. “This medicine is our bread and butter, but it didn’t help for us to eat while people were dying. We would be no better than HIV itself, killing people.”
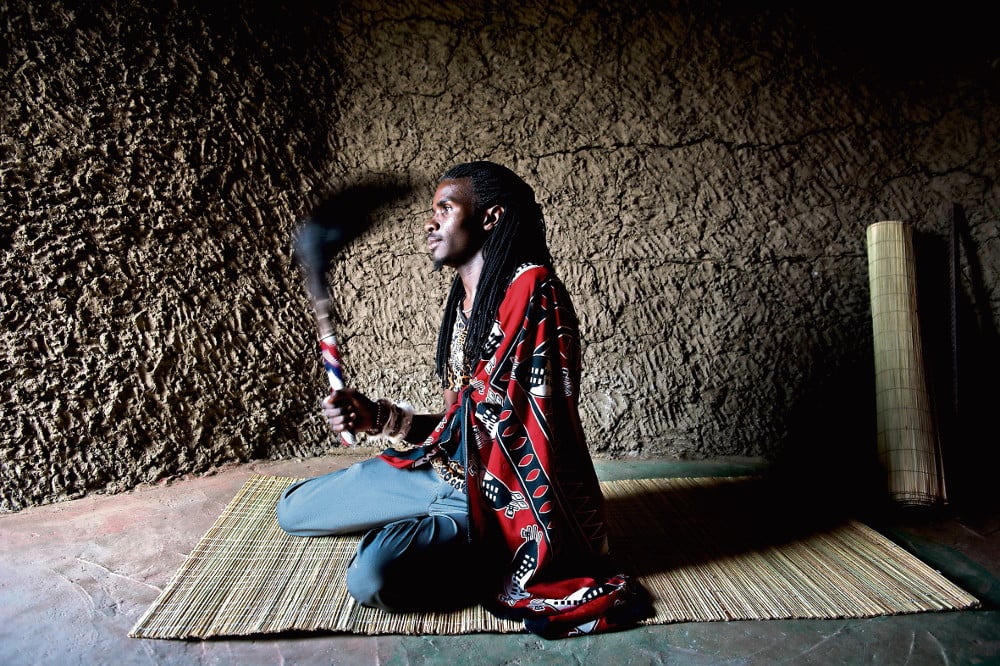 Healer Innocent Miya, a graduate of iTeach, lives on the banks of the Umlazi River
Healer Innocent Miya, a graduate of iTeach, lives on the banks of the Umlazi River
About 20km south of Memela’s home, Innocent Miya makes his way down a gravel footpath, the final part of the journey to his house in Hopewell. An old woman walks hunched over out of one of the mud houses. When she sees him she smiles, revealing toothless gums. They exchange greetings:
“eMakhosini!” she says.
“Makhosi!” Miya responds.
“That is one of my students,” he explains.
The 25-year-old traditional healer lives in a small house on the banks of the Umlazi River. A few metres from his house is a mud hut with a tin roof. This is where he consults clients and trains initiates. Miya is one of iTeach’s recent graduates.
The programme started in 2009 in Msunduzi, one of the local municipalities in the uMgungundlovu district. It has since expanded to include traditional healers from other municipalities in the district.
Deli Mthimkhulu is the project manager at iTeach. She is also in charge of training the traditional healers. “Our training programme consists of a three-day workshop that covers the basics of HIV and tuberculosis. From there we take them for a 10-day counselling course. After that they go through a four-week mentorship at the clinics where they have to complete 50 HIV tests before they graduate.”
Lives are saved when both systems are respected
Shortly after Miya completed his training with iTeach, one of his initiates got sick. He had sores on his face and on the soles of his feet. This prompted the healer to take the initiate to Edendale Hospital.
“During our training they showed us a picture of someone with blisters on their feet, so when I saw that I decided he needs to get a check-up,” he says. “There are some things that we cannot do with Zulu medicine that must be done with white medicine.”
Miya’s view is supported by a 2011 African Journal of Traditional, Complementary and Alternative Medicines article, which states that “to minimise the current distrust between modern and traditional doctors … both traditional and modern doctors must acknowledge their areas of strengths and weaknesses from which they operate”. The article further notes that “traditional healers have contributed to promoting positive health behaviour and serve as a good referral point to modern healthcare systems”.
This is contrary to a widely held belief that patients must choose between traditional practices and life-saving antiretrovirals (ARVs). The belief is “perpetuated by doctors and nurses who scold patients and tell them to stop taking traditional remedies … but this only causes patients to withhold information from their doctors”, Dong says.
 iTeach is run by director Krista Dong and Deli Mthimkhulu is in charge of training
iTeach is run by director Krista Dong and Deli Mthimkhulu is in charge of training
Vuyiseka Dubula, from the Africa Centre for HIV and Aids Management at Stellenbosch University, says the main concern about patients on ARVs using traditional medicine “are contra-interactions between ARVs and traditional medicines”.
According to a 2011 article in the journal Biopharmaceutics and Drug Disposition, those who use traditional, complementary and alternative medicines “in addition to antiretroviral treatment may be at risk of experiencing clinically significant interactions”.
Dong says her programme doesn’t “promote use of traditional medicine but it aims to systematise and make safer the dual care the patients are already obtaining”.
“We acknowledge that people are using traditional medicine and we try to make it as safe as possible and keep them informed. And we do that by informing the traditional healers so they really understand the HIV side. Not to change them, just so they know how to navigate their patients.”
Fifty-one percent of patients on HIV treatment who took part in a 2008 Human Science Research Council survey reported using traditional or complementary medicine such as multivitamins and immune boosters. Seeking both conventional and alternative treatments is a practice that is also seen in other countries. A 2007 study in western Uganda reported that 63% of participants turned to traditional medicine after being diagnosed with HIV. A 2013 study in Ghana found that 53% of HIV-positive participants used traditional medicine.
HIV training for patients
Back in a dimly lit room in Edendale Hospital, two elderly women speak to a small group of patients who have recently learnt they are HIV positive and will start treatment.
Dressed in navy skirts and baby-blue shirts with the iTeach logo, it is not easy to tell that these women are traditional healers. “Recap of modules”, reads an image reflecting on the wall from the overhead projector.
“The traditional health practitioners that we train provide a wide array of services, from literacy training to HIV counselling and testing. They actually train every single patient starting on ARVs here at Edendale Hospital,” Dong explains.
Mbali Ndlovu, the uMgungundlovu District Municipality’s spokesperson, says: “Traditional healers have been involved in delivering patient HIV literacy at Edendale Hospital since 2010, including ongoing counselling and defaulter counselling.”
Slindile Kunene (25) is one of the patients who received counselling from these traditional healers. “I first met the iTeach people at the Edendale Hospital. I was very sick and hospitalised, but I didn’t understand what was wrong until they explained it all to me. I was HIV positive. They taught me how to take my medication and told me to go to the clinic if I start feeling sick.”
When she fell pregnant in 2014, it was again the traditional healers stationed at Edendale Hospital who helped get her on to the hospital’s prevention of mother-to-child transmission of HIV programme. Today, her baby is HIV negative and Kunene is still on treatment.
 Slindile Kunene was counselled by traditional healers at Edendale Hospital
Slindile Kunene was counselled by traditional healers at Edendale Hospital
The Joint United Nations Programme on HIV and Aids estimates that there are 6.8-million people in South Africa who live with HIV. According to the 2014-2015 District Health Barometer, “469 000 new infections were recorded at the end of 2012, with particularly high incidence levels among young women aged 15–24 years. KwaZulu-Natal has consistently experienced the highest prevalence level among 15–49-year-olds at 37.4% in 2011 and 2012.”
Figures from the Provincial Aids Council indicate that uMgungu-ndlovu, which is also one of the National Health Insurance pilot districts, has the highest HIV prevalence in the province. The National Antenatal HIV Prevalence Survey estimates that 40.7% of pregnant women attending government facilities in 2012 were HIV positive.
Traditional healers: a ‘smart’ resource
“Engagement of traditional healers represents smart utilisation of an ‘available resource’, particularly in KwaZulu-Natal where healers are both trusted and abundant,” says Ndlovu.
Although the actual number of healers is not known, Ndlovu believes it is large. “The challenge is that there is no single point of registration for traditional healers, either at the district, provincial or national level,” she says.
An interim Traditional Health Practitioners’ Council has been developing a system to regulate and register traditional healers, according to the national health department.
To date about 300 traditional healers have gone through the iTeach programme and, as part of their training, performed roughly 14 000 HIV tests.
Ndlovu estimates that 10 000 patients went through the literacy training conducted by the traditional healers before starting on treatment.
“Traditional healers have participated in over 40 events sponsored by the health department in the last two years, at which [more than] 1 200 patients have been tested,” she says.
“HIV testing delivered by traditional healers has been received incredibly well at the local universities. iTeach-trained healers have been the official providers of HIV testing for the University of KwaZulu-Natal’s Pietermaritzburg campus, and have tested over a thousand students in the last two years. Testing of students by traditional healers is also provided at the Technical Vocation Education and Training college campuses, including their Edendale, Midlands and Plessislaer campuses.”
 Collaboration: Healer Senzikile Mbhele works full-time at iTeach
Collaboration: Healer Senzikile Mbhele works full-time at iTeach
Senzikile Mbhele, one of the six traditional healers who are full-time staff at iTeach, believes the reason this type of collaboration has not caught on in many parts of the country is a result of some healers who say that they can cure HIV.
The Africa Centre’s Dubula warns that, although “some traditional medicines have shown signs to treat opportunistic infections, they are not proven to cure nor treat HIV”.
Mbhele says only uninformed traditional healers will claim to cure HIV. “We know that it [HIV] penetrates areas that our medicine can’t reach. Yes, we can cure the opportunistic diseases and minor illnesses, but HIV is not curable.”
She says people opposed to traditional medicine simply don’t understand how it works.
“You can use traditional medicine without drinking it, to prevent it interfering with ARVs. You can have medication where you steam that doesn’t affect ARVs because it doesn’t go into the body. The whole point is to make sure that a patient doesn’t drink medicine that will interact with the ARVs. But traditional medicine works. It’s just that people have to be informed on how to use it,” says Mbhele.
“We can even initiate somebody who is on ARVs. We just have to find a way to initiate that is suited for them. For example, someone on ARVs can’t bathe in cold water or purge. So we will ask the ancestors that he does it differently so that his health is not compromised.”