Sex workers can take a pill that significantly reduces the risk of HIV infection.
Brandon Gacheru* (25) makes a living by having sex with people he hardly knows. He specialises in intercourse with other men. “I’m not always able to use a condom. And when I do, they sometimes burst,” he says. “Because I have multiple partners, I know I’m at risk of getting sexually transmitted infections.”
Gacheru lives in Kenya’s capital city, Nairobi. Sex work is illegal in his country. Yet in 2012, the East African country had 200 000 commercial sex workers, of which 15 000 were men, according to a survey by the National Aids and Sexually Transmitted Infections Control Programme and other partners.
A male Kenyan sex worker tells us how the HIV prevention pill has changed his life
[multimedia source=”http://bhekisisa.org/multimedia/2016-08-25-a-male-kenyan-sex-worker-tells-us-how-the-hiv-prevention-pill-has-changed-his-life”]
Gacheru has oral and anal sex with his clients. Kenya’s strategic Aids framework for 2014-2015 to 2018-2019 says only about three-quarters of men reported using a condom the last time they had anal sex with a male partner.
Anal intercourse without a condom makes men who have sex with men particularly vulnerable to contracting HIV: studies have shown it’s the riskiest type of sex for HIV transmission.
A 2010 study in the International Journal of Epidemiology suggests that the per-act probability or risk of HIV infection from unprotected anal sex is about 18 times higher than that of unprotected vaginal sex.
It’s possible for either partner — the insertive partner or the receptive partner — to get HIV, but it is much riskier for an HIV-negative partner to be the receptive partner.
Because of his job, Gacheru is often a receptive anal sex partner. “You can unfortunately not negotiate your way out of all risks,” he says. “Worse still, you can be raped.”

Brandon Gacheru* (25) is a sex worker in Nairobi, Kenya. (Kiundu Waweru)
Truvada – a pill to reduce HIV infection
Gacheru, who is HIV negative, is a peer educator at LVCT Health, a nongovernmental organisation that provides sexual health services and conducts research on preventing HIV. Here, he has learned about a pill called Truvada that he can take to reduce his chances of contracting HIV.
Truvada contains two ingredients, emtricitabine and tenofovir, which are used in antiretroviral medication that HIV-infected people take. Studies have shown that when the pill is taken once a day by an HIV-negative person, it can decrease the person’s chances of contracting the virus by more than 90%.
Late last year, Kenya became the second African country, after South Africa, to approve the use of Truvada as a form of HIV prevention, which is known as pre-exposure prophylaxis (PrEP).
PrEP is particularly useful to people who are at a higher risk than the general population of contracting HIV. The World Health Organisation has identified three such groups: men who have sex with men, young women (15- to 24-year-olds) and sex workers.
Organisations in Kenya are running demonstration studies investigating how best to deliver PrEP treatment to people who need it.
Gacheru is part of one such study, run by LVCT Health. This way, he gets his PrEP pills for free. The study is following 2 100 PrEP users across Kenya for a year to find out, among other things, whether they’re taking their pills correctly: each day at more or less the same time. The less often a PrEP user takes Truvada, the less effective it becomes. The pill also works better when it’s taken at a specific time each day.
Gacheru is one of the 250 male trial participants who have sex with men in Nairobi. He finds it difficult to take his pill at the same time every day. “I take my medication at 11pm each night. But sometimes I am out clubbing during that time and don’t have a pill with me,” he says. “I rarely carry a Truvada pill with me for fear of stigma. People won’t believe I’m taking it for prevention. They will think I am HIV positive.”
The dos and dont’s of using an HIV prevention pill
[multimedia source=”http://bhekisisa.org/multimedia/2016-04-06-the-dos-and-donts-of-using-an-hiv-prevention-pill”]
The MemsCap monitoring system
Gacheru receives a month’s supply of Truvada in a vial with an electronic cap called a MemsCap. Mems is an acronym for medication events monitoring system. The cap has a digital monitor that makes an electronic note every time it is opened and a pill is removed.
Gacheru has to check in with trial researchers once a month. His MemsCap is refilled and he is tested for HIV. But before he receives the next month’s supply, the researchers download the information stored in the MemsCap using specialised software. It analyses Gacheru’s adherence and generates a graph showing the date and time at which each pill was taken.
LVCT research manager Jordan Kyongo says that in instances where a patient opens the vial but does not take the pill, doctors could perform intermittent blood tests that show how much Truvada is in the person’s system.
The MemsCap system has been used by more than 500 000 patients in over 70 countries in the past 20 years, according to Bernard Vrijens, who works for the Aardex Group, which manufactures the caps. He says apart from Kenya, other countries using the MemsCap to test adherence to PrEP include Nigeria, Senegal and India.
Vrijens says the MemsCap system “helps healthcare practitioners understand the behaviour of their patients, which is important in designing interventions.
“The use of the MemsCap varies from clinical trials to measuring adherence of new medicines in diverse fields, from hypertension and oncology to depression and HIV. Some of the results from these projects are contained in 700 peer reviewed journals,” says Vrijens.
He says PrEP is a “life-changing medical intervention in the battle against HIV” but the “war” can only be won when people adhere to the prescribed drug regimen.
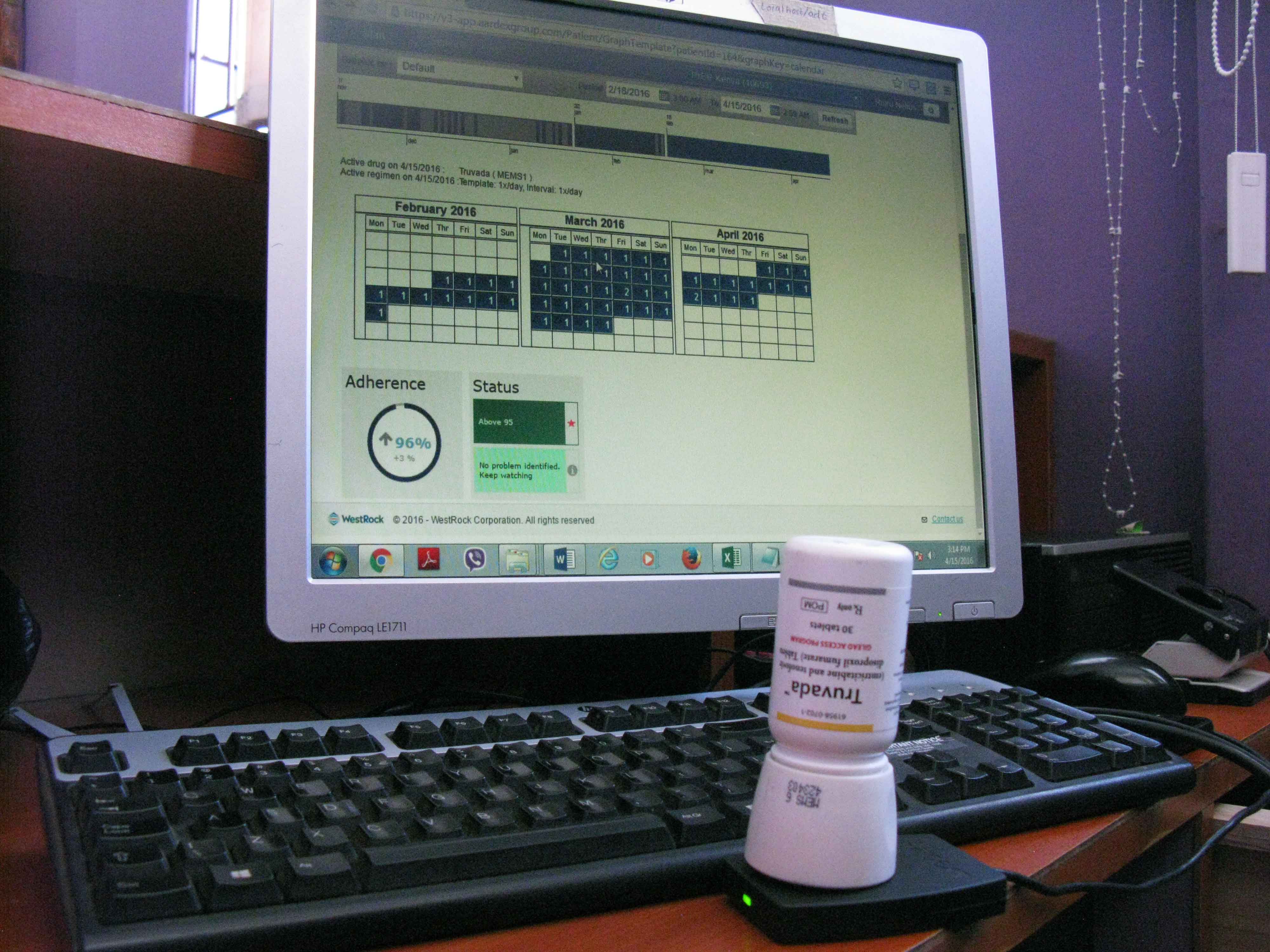
The MemsCap, an electronic cap used to monitor Truvada users pill consumption. (Kiundu Waweru)
Going ahead with PrEP
The results of the study in which Gacheru is a participant will be available in April 2017.
A study published in April in openaccess journal PLOS ONE, which surveyed 80 men who have sex with men in Kenya, found that 83% of them were willing to take a daily PrEP pill.
The Kenyan government is drafting clinical guidelines for doctors on how to use PrEP. According to Helgar Musyoki, the key populations programme manager at the country’s National Aids and Sexually Transmitted Infections Control Programme, the guidelines will be released on July 14.
“The pill will [eventually] be available at government facilities [to high-risk groups], although the draft guidelines propose that it should also be provided over the counter [at pharmacies],” Musyoki says.
“But no person will be able to get access to Truvada [or a generic] without a prescription from a health professional. It is not a ‘magic bullet’ and has to be taken as a package with other preventive measures.”
Back at his flat in Nairobi, Gacheru is getting ready for the night’s work. Because of stiff competition in the city, he uses a mobile phone application, Grindr, which helps him check out profiles of potential clients. It also provides the real-time location of users.
Most importantly, Gacheru says, the inbox feature of the app allows him to negotiate terms such as the use of protection before he meets up with prospective clients.
“But it’s simply not always possible to have safe sex. When I can’t use a condom, I’m very grateful to also have access to a pill that protects me against HIV infection. But I have to take that pill every day, condom or no condom.” — Additional reporting by Mia Malan.
* Not his real name