Two decades and three South African Human Rights Commission investigations later
It’s a May morning in 2018 and cancer activists, journalists and politicians are seated around a fluorescent-lit conference room at the offices of the South African Human Rights Commission (SAHRC) in Braamfontein, Johannesburg.
A lone broadcast camera is angled towards the table in the centre of the room and representatives of the KwaZulu-Natal health department take their seats, flanked by their legal team.
The department’s acting head of health and chief executive of Durban’s Inkosi Albert Luthuli Central Hospital nervously set up their computers. It’s been almost a year since Durban lost its last state oncologist and more than two years since the SAHRC began investigating collapsing cancer services in the province.
But someone is missing.
KwaZulu-Natal’s health MEC Sibongiseni Dhlomo. The honourable MEC will be late, his legal counsel explains.
“Unbelievable,” tuts a disgruntled Imran Keeka, the Democratic Alliance’s spokesperson for health in KwaZulu-Natal. It was Keeka’s complaint to the SAHRC that launched an inquiry into the province’s oncology services. The commission would later find that the health department violated cancer patients’ right to health by failing to care for them.
It would be another two years before Dhlomo appeared before the commission at their Johannesburg office block, earlier this year. By that time, at least 500 cancer patients had died in state hospital beds awaiting treatment.

The SAHRC was established in 1995 under the Human Rights Commission Act to promote, protect and monitor human rights. The commission is one of eight bodies established in terms of Chapter Nine of the Constitution.
Under the Act, the commission has the power to investigate human rights violations, subpoena people to appear before it and make recommendations for redress although these aren’t legally binding. The body can, however, sue parties that don’t implement recommendations, says Sasha Stevenson, the head of health at legal nonprofit Section27.
In recent years, the human rights commission has received complaints about everything from a lack of mobile clinics to KwaZulu-Natal’s crumbling cancer services. Headlines decrying the state of South Africa’s public health sector have reached a fever pitch, leading citizens and opposition parties alike to turn to the SAHRC. But the commission’s health investigations have yielded mixed results. As the body navigates a new terrain of scarce funds and an uncertain future, some organisations are placing their hope in the country’s new health ombud.
The commission investigated several major health inquiries – three in the last two decades – into conditions at Lindela Repatriation Centre for undocumented migrants. The body found that officials at the Krugersdorp facility outside Johannesburg denied detainees proper nutrition and adequate access to HIV and tuberculosis (TB) medicine. Meanwhile, the commission found that overcrowding at Lindela made conditions there ripe for the transmission of TB.
Similarly the watchdog has twice interrogated the availability of ambulances – nationally in 2007 and in the Eastern Cape in 2013. The commission found the province violated patients’ right to emergency medical care by providing less than half of the vehicles required by national health department standards.
Guidelines say there should be one ambulance for every 10 000 people. The Eastern Cape had just 300 working ambulances when the SAHRC began its investigation, a 2015 commission hearing report showed.
Section27 is part of the civil society Eastern Cape Health Crisis Coalition, which was a complainant in the Eastern Cape hearing. In the two years since the commission’s hearing report, Stevenson says there have been some improvements.
The provincial health department has bought 140 new ambulances and eradicated the understaffed “one-man” ambulance crews as the commission recommended.
“An ambulance with only a driver is just a taxi with a stretcher. You need someone to provide care while you’re going,” she explains.
But Stevenson argues the province’s emergency medical services are still inefficient.
“You can call an ambulance, and it might come. But only four to six hours later,” she says.
“You still can’t rely on the system.”
The commission’s recommendation that the province trains rural community members to provide first aid at least in the absence of better EMS has gone unimplemented.
Stevenson says when the commission was asked why it had not done more to track whether the province had acted on its recommendations, its Eastern Cape office said: “We didn’t have the budget.”
 Health conditions at Lindela Repatriation Centre for undocumented migrants remain dangerous despite South African Human Rights Commission investigations spanning two decades. (Paul Botes)
Health conditions at Lindela Repatriation Centre for undocumented migrants remain dangerous despite South African Human Rights Commission investigations spanning two decades. (Paul Botes)
Starting this year, the treasury will slash the commission’s budget by about R5-million annually until 2021, according to treasury data. This leaves only R3.2-million for the SAHRC to fulfil its constitutional mandate in 2018, the commission’s spokesperson Gail Smith, says. Money for investigations, hearings, litigation and human rights monitoring are all paid from this purse. Chief executive Tseliso Thipanyane says treasury told the commission that the cuts were partly to fund free higher education.
Funding to implement the National Health Insurance (NHI) scheme will also increase by more than R4-billion until 2021, treasury data shows.
Thipanyane explains: “We are a small organisation. Almost 75% of our budget goes to salaries.
“If nothing changes, we could be forced to retrench.”
Thipanyane says the government could be deliberately strangling the body. “Those who exercise power typically do not want to be held to account.”
The Chapter Nine institution’s shrinking budget is not enough to prove it is being stifled. Cabinet also approved R85-billion in budget cuts this year across all government departments, says treasury spokesperson Zwikhodo Singo.
Alison Tilley, the head of advocacy at the social and economic justice nonprofit the Open Democracy Advice Centre, argues that the way commissioners are recruited is a bigger worry than inevitably shrinking budgets.
The ANC’s deployment committee vets candidates before their appointment to senior positions in Chapter Nine institutions.
“That in itself is a strangling of these institutions. Candidates should not be vetted by the majority party,” she says
Uncertainty about what the future holds for Chapter Nines could also be keeping the watchdogs on a leash, Tilley says. In 2007, a committee led by late ANC stalwart Kader Asmal recommended that five of the eight institutions be merged into one human rights protector.
But more than a decade later, no plans have been announced. “There is no clarity on where these institutions will be five years from now,” Tilley warns.
Meanwhile, the number of public complaints regarding violations of the right to health has increased by nearly 45% since 2016, according to SAHRC annual reports. The commission received 641 such complaints in 2017, second in number only to those regarding equality.
By comparison, the recently created Office of Health Standards Compliance (OHSC) received at least 730 complaints in the first eight months of establishing a national call centre, according to the OHSC 2016/17 annual report. The OHSC and its ombud were created in part to monitor the quality of health services. The flood of calls followed the health ombud’s high-profile investigation and damning report on the Life Esidimeni tragedy in which 144 mental health patients lost their lives after being removed from long-term, state-funded care at private Life Esidimeni facilities.
The ombud – and not the commission for a change – may also be the latest to take over investigations into health services at the Lindela Repatriation Centre.
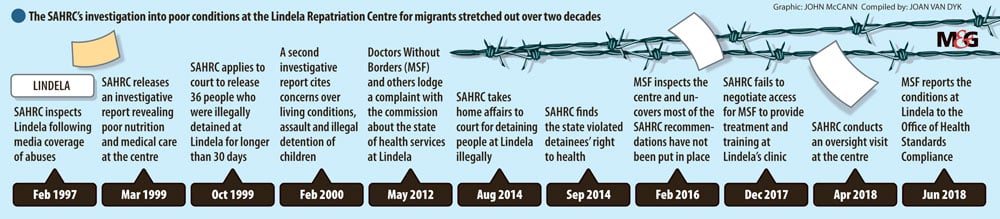
Over the past 15 years, the commissions’ many investigations into Lindela have uncovered not only inadequate medical care at the facility but also the illegal detention of migrant children. Complaints filed by the public interest litigation organisation Lawyers for Human Rights (LHR) and international humanitarian organisation Doctors Without Borders (MSF) prompted a 2012 interrogation at the centre. Subsequently, the pair gained very limited access to Lindela to conduct oversight visits through the commission. Almost half of 35 recommendations made by the trio to improve health services and conditions at Lindela have not been implemented, according to a 2017 MSF document.
After witnessing the dire conditions at Lindela, MSF proposed to station a medical team at Lindela’s clinic. The group would train doctors and nurses at the clinic to assess detainees for TB, HIV and other conditions.
“Proper screening is needed to ensure the clinic is not illegally admitting children – none of this is happening at Lindela,” MSF medical co-ordinator Amir Shroufi told Bhekisisa in December 2017.
South Africa’s own national strategic plan on HIV and TB requires that the country prioritise ways to stop TB transmission in detention settings. The strategy also calls for greater co-ordination between southern African countries to ensure that migrants can access HIV care. South Africa already provides HIV and TB medication to anyone in the country regardless of documentation.
But MSF’s proposal relied on the commission negotiating access to Lindela on its behalf. Ultimately, it failed to do so.
In December, Smith said that although the commission was supportive of MSF’s aims, they were “not fully aligned with the monitoring focus and support envisaged by the Commission”.
She added that the need for the commission to “present its own concerns to the new political leadership of the department” also impacted on its ability to get approval for MSF to access the facility long-term. At the time, the department of home affairs had just undergone its fifth change in minister in as many years.
As a result, MSF has now turned to the OHSC, submitting a complaint about care at Lindela in late June.
“The OHSC has acted decisively in the past where there has been a lack of oversight – this is needed for the clinic at Lindela,” says Garret Barnwell, who was part of the MSF team that conducted the latest assessment of Lindela.
In 2016, the health ombud Malegapuru Makgoba released a damning report into the circumstances around the deaths of almost 100 mental health patients who had been removed from state-funded private Life Esidimeni healthcare facilities. Stevenson argues that the success of Makgoba’s intervention is a prime example that state watchdogs’ effectiveness depends on the quality of their leadership – and the willingness of government leadership to respond.
At least 144 patients died as part of the Life Esidimeni tragedy. Families of 135 patients involved were awarded R1.18-million in damages as part of the arbitration. The National Prosecuting Authority is still considering possible criminal prosecutions related to the doomed move.
The SAHRC received a complaint about the transfers in March 2016, but did not respond until August, just weeks before former health MEC Qedani Mahlangu disclosed that 36 mental health patients died at mostly unregistered nonprofits. A subsequent ombud report would reveal that the actual death toll was almost double that at the time when Mahlangu presented the data to the Gauteng provincial legislature.
“Lives could have been saved if the commission acted seriously,” the DA’s shadow health MEC in Gauteng Jack Bloom said in a 2017 statement. The SAHRC has since appointed a new commission for health matters.
Although Thipanyane admits the Commission has not sufficiently followed up on recommendations it has made in the past, Smith argues government’s failure to comply with them is the real threat to the commission’s effectivity.
But when state departments refuse to implement recommendations – whether about ambulances, detention facilities or even KwaZulu-Natal’s current cancer crisis – both Stevenson and Smith say going to court isn’t always the answer.
The body has increased its litigation efforts by 32% since 2013. In 2016/17 alone, the SAHRC instituted 62 new litigation cases.
But legal action can take years to finalise and budget constraints force the commission to tread carefully before using scarce public resources, Smith says. The commission’s CEO Thipanyane admits the body will likely avoid the courts in future to accommodate a smaller budget.
“We can’t spend two years in courts to deal with a single human rights violation. We just don’t have the money.”
 Beauty Zulu, a cervical cancer patient, was forced to wait months when oncology services in KwaZulu-Natal ground to a halt in 2016. (Madelene Cronje)
Beauty Zulu, a cervical cancer patient, was forced to wait months when oncology services in KwaZulu-Natal ground to a halt in 2016. (Madelene Cronje)
At the commission’s May hearing into collapsing oncology services in his province, KwaZulu-Natal health MEC Sibongiseni Dhlomo finally came face-to-face with commissioners. He had been subpoenaed to appear after repeatedly failing to meet SAHRC deadlines to improve oncology care in the province.
In a three-hour hearing, the man responsible for health in the province testified for about 10 minutes.
The health department bombarded the commission with data at the last minute, says the main complainant and DA MPL Imran Keeka. This, he claims, allowed Dhlomo to divert the conversation to issues that had already been resolved.
“It’s worrying that they failed to question him properly,” Stevenson says.
Although it may be time consuming and expensive to use the might of the law, the SAHRC – and other Chapter Nine institutions – have huge powers to request information and conduct inspections.
“It’s easier to get to the bottom of things through the Commission than through the courts,” she says.
There are no guarantees in court: “As the person bringing the case, you have to hope the other side provides information that will be useful to you.
The commission will now compile a hearing report, which in the case of the Eastern Cape EMS hearing took about six months.
In the case of KwaZulu-Natal’s oncology collapse, the Commission was bound by its own policies to give the department sufficient time to redeem itself after it failed to meet the watchdog’s deadlines.
“Seeking redress for human rights violations takes time,” Smith says.
The party is now also expected to turn to both the OHSC and public protector in a bid to help solve KZN’s oncology emergency but also other health crises across the country.
“We encouraged the commission to prosecute but that wasn’t done,” Keeka says.
“We want to see justice done for the families of those that have died in the crisis, which MEC Dhlomo has presided over.”