A medical worker wearing personal protective equipment (PPE) collects a nasal swab sample at a walk-in and drive-thru coronavirus testing facility in Pretoria. Photographer: Waldo Swiegers/Bloomberg via Getty Images
Although Omicron has spread rapidly and replaced other variants in a shorter period, preliminary data shows that individuals who contracted the variant were 80% less likely to be admitted to hospital, while those who did end up in hospital were also 70% less likely to develop severe disease.
When compared to the third wave, where the severity rate on those who were admitted with the Delta variant was at 65%, only 32% of cases admitted with the Omicron variant were severe.
Scientists at the National Institute for Communicable Diseases (NICD) say that the lower severity rate of Omicron is an indication that future variants from Covid-19 are more likely to have a similar outcome.
The average hospital stay during the third wave was six days. This has come down to only three days in the fourth wave. About 821 people who were admitted during the fourth wave died in hospital compared to 3 575 in the third wave.
“We are likely to enter the next wave in a better position with even higher seroprevalence and immunity from both natural infection and vaccination. I think it’s now a move towards the virus becoming more endemic where we will likely see these waves become smaller as the whole population protection increases,” said the NICD’s Dr Michelle Groome during a virtual briefing held by the institute on Wednesday.
Groome also added that people who had been infected before were probably infected again during this wave and had therefore had their immunity boosted.
“We are in a situation where people have had prior infection, they have had vaccination and if we increase our vaccination rates, that will provide a boost,” she added.
Professor Cheryl Cohen agreed that previous exposure as well as vaccination provided protection against severe disease.
According to Cohen, population immunity would kick in over time as more and more people got vaccinated or had a previous infection. This trend, which has been seen with other viral infections like influenza, was expected to continue with Covid-19 and that it would become an endemic infection over time Cohen explained.
A preprint of their paper, which has not been peer reviewed yet, states that by November a high proportion of the South African population had some level of Covid-19 immunity, as a result of previous natural infection or vaccination.
In the paper it is estimated that 60% to 70% of South Africans had evidence of a previous infection by the end of the third Covid-19 wave. It further broke down the vaccination rates among age groups by 9 December, saying 58% of people aged 60 and over, 55% aged 50-59 years, 43% aged 35-49 and 24% aged 18-34 years were fully vaccinated with one dose of Johnson & Johnson (J&J) or two doses of the Pfizer vaccine.
The study found that the data compared to earlier Delta infected individuals, suggests that this reduced severity may be in part be a result of high levels of population immunity.
However, the authors do warn that the analysis was conducted in the early phase of the fourth wave after the emergence of Omicron when numbers were small and patients with milder symptoms were more likely to be admitted, so there may be a lag in hospitalisations and severe outcomes caused by this new variant.
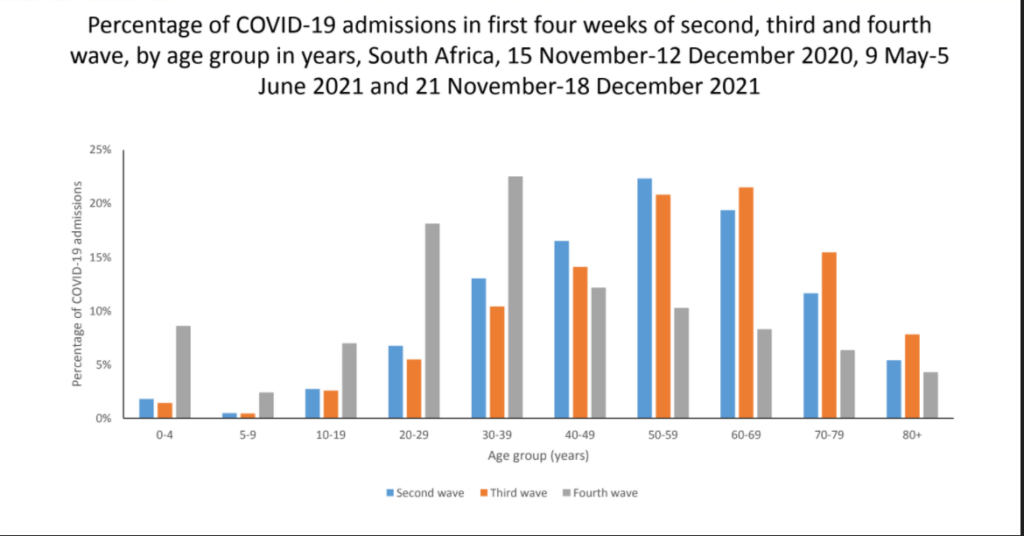
Meanwhile, a joint scientific mission to study the Omicron variant between Russian and South African scientists, which was conducted from 13 to 22 December, found that there was a high incidence of Covid-19 infection among children in the initial stages of the variant, where up to 50% of all patients seeking medical care for various reasons were infected.
There were also clinical characteristics of influenza among those who were infected, a large number of infections were asymptomatic and the population seroprevalence reached up to 70%.
Omicron was also found to have been more severe in unvaccinated people with risk factors, especially in older age groups. Data collected between 7 November to 18 December by the NICD showed that from the 309 Covid-19 hospital deaths, 40 of them were fully vaccinated while 269 were unvaccinated or not fully vaccinated. Nine of the deceased had received one dose of the J&J vaccine, 28 had a single dose of the Pfizer vaccine while 35 had received two doses.