Daydreams of a health minister: The high-level meeting on TB this week in New York is in part the work of Health Minister Aaron Motsoaledi. (Reuters)
It’s finally here. After months of negotiations, at least one international spat and what we are sure are countless of track changes later the world finally has its first United Nations declaration on TB.
Heads of state, including our own President Cyril Ramaphosa, will ratify the declaration this week at the UN’s first high-level meeting on TB in its 73-year history.
And boy, has TB bided its time. TB is single deadliest infectious disease today, World Health Organisation figures show.
The ink’s mostly dry on the 16-page declaration, which you can check out below, but activists are expecting countries, including the United States, to capitalise on the meeting to make some major announcements. Our Laura Lopez Gonzalez explains:
We’ll be live blogging from the Big Apple to bring you the latest here and on Twitter @Bhekisisa_MG. And don’t forget to subscribe to our weekly newsletter.
10:56 am 27 September: The final body count
In our interview with MSF Access Campaign HIV and TB advisor Sharonann Lynch ahead of the meeting, she called out heads of state including those from high-burden TB countries such as India and China for failing to show up for the meeting.
StopTB Partnership had expected 32 presidents and prime ministers to show up to the world’s first UN meeting on TB.
The final count: Less than 30, according to Lynch in a statement.
“Shame on the more than 160 leaders who were absent,” she explained.
“But just because the cameras are off and leaders have stepped off the world stage doesn’t mean they can return to business as usual. They have to take advantage of this momentum and truly commit to significantly increasing investments and mobilizing the research community to develop new medical tools to more effectively tackle the world’s deadliest infectious disease—for the 10-million people who develop TB each year still desperately waiting for a fast, safe, and simple cure.”
Only 10 leaders showed up to the last high-level meeting on HIV in 2016, StopTB Partnership deputy executive director Suvanand Sahu told Bhekisisa earlier this week.
The struggle is real. Lynch tweeted about “promises fatigue” during the meeting because sometimes you want to be like “heeeyyyy” to leading TB research experts.
But then sometimes you’re like “World, stop toying with my emotions” and the lives of millions.
1:00 am 27 September: Read President Cyril Ramaphosa’s full remarks at the UN’s first ever high-level meeting
The National Health Insurance and the fight against the leading cause of death in the country, TB, are inextricably tied, Ramaphosa says.
Ramaphosa was speaking at the launch of the world’s first UN declaration on TB, which coincided with the global body’s general assembly in New York.
“This first-ever UN high-level meeting on tuberculosis is a historic opportunity that we must embrace if we are to effectively respond to a disease that has killed more people than smallpox, malaria, the plague, influenza, HIV and Aids and Ebola combined”, the president explained.
The meeting is done and dusted, now activists will be looking to see how to best track country progress on the declaration.
Read Ramaphosa’s full remarks:
12:04 am 27 September: It’s a wrap. For now.

The UN’s first high-level meeting on TB is done and dusted. The world now has a UN declaration on the deadliest infectious disease in the world. Now, the world will watch to see if countries will keep their promises.
Here are some parting words from the meeting chair:
“The level of interest in this meeting was much greater than the minutes we had in this day. Around 45 states were not able to take the floor and six observers were in the same position. Thank you once again for the enormous interest and participating in this first high-level meeting on TB.
“When we opened this meeting, we had two objectives: One was more ambitious – to bring an end in TB. The second was to agree on a political declaration. I am particularly happy that we reached our immediate goal.
“But what is the next step? We need to ensure that our leaders and the private sector invest the necessary resources. commitments have been made, the plan is on the table. The only thing left is to act.”
11:35 pm 26 September: Leave no one behind
Ahead of the meeting, it was clear that the world needed to do better about diagnosing, treating and preventing TB. But who should the world be focus on reaching was a matter of debate with so many people at risk: Children, men, miners, people living with HIV.
Ultimately, the declaration recognised the following vulnerable groups by name:
- women
- children
- indigenous peoples
- health care workers
- migrants
- refugees
- internally displaced people
- people living in situations of complex emergencies
- prisoners
- people living with HIV
- people who use drugs particularly those who inject drugs
- miners and others exposed to silica
- urban and rural poor
- underserved populations
- undernourished people
- individuals who face food insecurity
- ethnic minorities
- people and communities at risk of exposure to bovine tuberculosis
- people living with diabetes
- people with mental and physical disabilities
- people with alcohol use disorders
- people who use tobacco
Now, more than 130 civil society organisations representing these groups have put out a statement urging the declaration to go further. Check it out below, care of the Global Fund Advocates Network.
11:01 pm 26 September: Not to be outdone, UK makes it rain…
Well, sort of. Just hours after the US announces millions in new TB funding, the United Kingdom pledges £7-million (or about $9.2-million) in funding to the TB Alliance, which takes a unique approach to developing much-needed new TB drugs.
Here’s why the TB Alliance is important.
TB treatment is always given as a combination of drugs to help reduce the chances that patients will develop drug resistance. Normally, drugs are developed one at a time. But this means that when they are finally approved for use, they have to go back into clinical trials to be tested as part of combination therapy.
Translation: Developing drugs for TB one at a time takes a lot of time, time that patients don’t have considering the dearth of new medications invented in the last century.
To speed things up, the TB Alliance develops drugs in tandem, testing them out as regimens. This means the world gets new combinations of drugs faster, in theory.
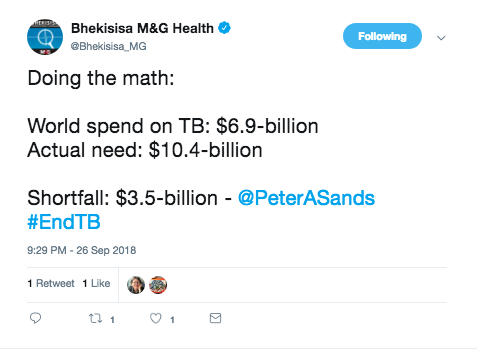
9:29 pm 26 September: Math interlude
Some interesting sums by Peter Sands, head of the international financing mechanism The Global Fund to Fight Aids, TB and Malaria.
9:15 pm 26 September: The fight that just won’t die
In case you just joined us, let me catch you up to speed. But first some background: More than a year ago, South Africa’s health minister Aaron Motsoaledi joins with other ministers from countries such as Brazil and Indonesia to get the UN to hold its first high-level meeting. At the meeting, the global body will launch its first ever declaration on the infectious disease.
For months ahead of this week’s meeting, policymakers work to fine tune drafts before a 20 July version pops up.
Spoilers: The July document puts forth a position championed by the US (although other countries may have supported it) that is accused of bowing to Big Pharma pressures. It waters down language around Trips flexibilities — basically, tools countries can use to challenge conventional patents to ensure access to affordable medicines.
Instead, the text has a sentence that reads:
“[We recognise] that intellectual property rights are an important incentive in the development of new health products.”
South Africa and many developing countries in the G77 are like:
via GIPHY
South Africa protests, locks horns with US and a compromise is reached.
Earlier today, President Cyril Ramaphosa re-states his support for Trips.
Then this happened…
Alex Azar is the US secretary for health and human services.
The shade.
It did not go unnoticed.
And then
Still not sure what Trips flexibilities are? Basically, they are internationally-sanctioned ways that countries can challenge conventional patent systems for the public good. The US, in fact, threatened to use them in 2001 when it needed large amounts of patented antibiotics it couldn’t afford in the face of chemical warfare threats.
Want to know more. This is a great explainer by UNAids.
We’ll just leave this here…
via GIPHY
8:56 pm 26 September: Speaking of cash money – US announces millions in new TB funding
Activists had been expecting a number of big announcements to coincide with the meeting and this was one of them. The United States’ development aid arm, USAid, has just unveiled its new Accelerator programme:

USAid head Mark Green explains more about what the accelerator is:
We are pleased to announce a new innovative global accelerator programme to end TB that will increase our support to government and local partners. The accelerate is a new business model that will catalyse resources across all sectors, first through a performance-based measurement system that will maximise investments in both the public and private sectors to allow us to better align our own funding with partner country commitments.
India will be among the first countries to receive $13-million worth of new US funding through the mechanism.
Find out more from this just-released briefing paper:
7:00 pm 26 September: We’ll be taking a short break so grab the popcorn — or the tissue
We’ll be taking a two-hour break as the meeting adjourns so sit back, relax and refill the popcorn. Better yet, check out this exclusive piece written by Motsoaledi about how he finally got the world to talk about TB.
Me, I am still recovering from the video message from Chinese First Lady China’s first lady Peng Liyuan in which she recounts how one doctor spent 20 days walking mile after mile to reach TB patients cut off after an earthquake.
No, you’re crying.
6:07 pm 26 September: The fight for TB and the National Health Insurance are inextricably linked, Ramaphosa says.
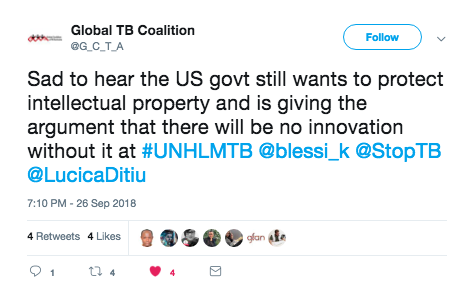
The only BRICS head of state slated to speak today, President Cyril Ramaphosa gives a recap of South Africa’s TB response.
But he says it will be impossible to end TB without a move to universal healthcare, or what in South Africa is known as the National Health Insurance. Read why:
“We need to ensure drugs are affordable, we must adhere to TRIPS flexibilities & ultimately all our efforts will not succeed unless we implement universal healthcare… those most affected by TB are also who have the greatest difficulty in accessing care.”
Ramaphosa has also reiterated South Africa’s position on Trips flexibilities or the rights of countries to challenge conventional patent protection on medicines on public health grounds. This has been a hugely contentious issue between the US and South Africa in the run-up to the meeting. South Africa has been pushing for greater recognition of patent flexibility for the public good for months now against US opposition. The final declaration is a compromise btw the two countries. (Get the backstory here).
So a loaded mention from the president as US Health and Human Services Secretary Alex Azar. StopTB Partnership deputy executive director Suvanand Sahu had expected 32 heads of state to attend the high-level meeting.
The last similar UN gathering for HIV in 2016 drew just 10, he told Bhekisisa.
Check out Ramaphosa’s full remarks:
4:30 pm 26 September: And we’re live!
The UN’s first ever high-level meeting on TB has begun. Watch it here. Motsoaledi opens the meeting by reviewing the declaration’s key provisions or “asks” and adds two more of his own:

Read the minister’s full remarks here:
11:05 am 26 September: Activists release alternative declaration
We’re just hours away from the official signing of the TB declaration. The document is a product of more than two months of heated negotiations, meaning the words on the page changed quite a bit to accommodate even issues you wouldn’t normally think impact an infectious disease — such as trade. (See more on that here and some useful background on trade and access to medicine here)
Here what we know was ultimately cut from the final version:
| What’s left unsaid: Some of the others issues that didn’t make it into the final draft |
| 1. National targets, including specific goals for high-risk populations such as prisoners, miners or children |
| 2. Commitments to putting national targets on paper in the form of strategic plans |
| 3. Timelines for new innovations such as shorter, pill-based regimens for all forms of TB, rapid tests and vaccines |
| 4. An independent accountability mechanism outside the UN system — possible including the World Health Organisation — to ensure future engagements from heads of state |
| 5. National R&D; funding targets. Dubbed the “Fair Shar Targets” this would have ensured that .1% of national research funding would have gone to TB |
But there’s more, say activists from advocacy organisations such South Africa’s Section27, Kenya Legal & Ethical Issues Network on HIV and Aids, and the Treatment Action Campaign.
Here’s what they think the declaration should have said:
Tuberculosis is a global emergency that kills over one and a half million people every year. It is the leading killer of people with HIV. Yet, collectively we have failed to respond effectively to TB because it mainly affects poor people including criminalised and marginalised communities such as people who use drugs, prisoners and their communities. We recognise our collective and individual failures. With this declaration, we make it clear that the old ways are not and never were good enough.
1. We commit to putting the money needed for TB research and for TB programmes on the table.
2. We commit to implementing and aggressively scaling up access to the latest evidence-based health technologies and policies in our countries. In short, we commit to ensuring that every single person who has TB receives the best available testing, treatments, and support – irrespective of their ability to pay or in which country they may live. In pursuit of this goal, we place human rights, and particularly the right to health, ahead of private interests and short-term political considerations.
In particular, we will take the following concrete steps:
3. Implement all World Health Organization (WHO) guidelines relating to the diagnosis, prevention, treatment and care of TB immediately but no later than six months after publication of such guidelines. We will ensure the rapid rollout of lifesaving new diagnostics such as [urine-based] LAM testing, and better and safer medicines such as bedaquiline. We commit to stop using medicines that do not work or worsen health outcomes for people with TB.
4. Establish ambitious national coverage and mortality reduction targets that ensure a bold scale-up of national efforts to address TB. These targets must be reflected in national strategic plans developed by countries in order to ensure effective accountability. These targets should include a) a reduction in mortality by 75% by 2025; b) a reduction in new infections by 50% by 2025; c) that 90% of people with TB will be diagnosed using WHO recommended rapid diagnostics by 2023; and d) that 90% of people with TB are able to access treatment by 2023 including newer, better and safer regimens for people with drug-resistant TB.
5. Commit to raising the money needed to close the funding gap to ensure a comprehensive response to the TB crisis, as outlined in the WHO Global Tuberculosis Report 2018. In 2018, investments in TB prevention and care in low- and middle-income countries fell US$3.5-billion short of what is needed. The annual gap will widen to US$ 5.4 billion in 2020 unless additional funding is committed. We will work collectively to establish an equitable funding formula for additional funds needed based primarily on countries’, including donor countries’, ability to pay.
6. Invest at least 0.1% of our national gross expenditure on research and development (GERD) on TB research starting in 2019 and we will continue with TB research investment at least this level until 2030. It is only through such a concrete, measurable commitment that we will ensure the annual US$2-billion that is required for TB research. We will ensure that TB health technologies developed with public and charitable funds will be equitably and affordably accessible to people with TB globally. We commit to ensuring that publicly-funded TB clinical trials include pregnant women, children, and people taking other treatments for HIV and other diseases and conditions. We commit to ensuring that better, more tolerable treatment regimens and co-formulations are developed at product development stages.
7. Implement the recommendation of the United Nations Secretary General’s High-Level Panel on Access to Medicines and establish, before the end of 2019, a binding convention on the research and development of critically needed health technologies for TB and other areas of urgent public health need. We commit to making annual financial contributions to a fund that will be established through the convention. We commit that no exclusive rights, in the form of intellectual property or any other means, will be granted on any products resulting from research funded through the convention.
8. We will, each country individually, by 2021, adopt, use, and protect the public health flexibilities available under the World Trade Organization (WTO) TRIPS Agreement as clarified by the Doha Declaration on the TRIPS Agreement and Public Health of 2001. We will raise the bar for patentability (excluding new uses, new forms, and new formulations of existing health technologies from patentability) and set up easy-to-use compulsory and government use licensing procedures with wide grounds for the issuing such licenses. Least developed countries will adopt the pharmaceutical transition period until 2033 or such time as they are no longer an LDC in accordance with the extension period allowed under WTO rules. We will, each country, refrain from any and all efforts in trade agreements or otherwise to impose TRIPS-plus measures or to retaliate or threaten to retaliate against other countries for using such measures.
9. We will, all high-TB burden countries individually, ensure rapid registration of TB health technologies. We commit to do this by making better use of the WHO’s Collaborative Registration system in order to speed up national registration processes, and, by facilitating and incentivising broad and expedited registration of TB medicines, diagnostics, and vaccines by originators and generic producers.
10. We will, all high TB-burden countries individually with the financial support of wealthy countries, fully fund aggressive contact tracing and active case finding campaigns in all high-burden countries to find the “missing people” with TB and ensure that TB is diagnosed and treated earlier, and implement programmes to ensure people are supported through treatment better. This will not only support the health of people with TB but also reduce the spread of TB in our communities. We commit to hiring the adequate numbers of health workers needed to scale up these campaigns in order to reduce TB mortality, and we agree to motivate them with a living wage, the tools and training they need to do their work, and the infection control they require.
11. We will, all high-TB burden countries individually and with the financial support of wealthy countries, conduct annual audits of TB infection control in all healthcare facilities, prisons and other public buildings where people gather in our countries. We commit to making the detailed results of these audits publicly available together with turnaround plans based on the challenges identified to address shortcomings in infection control.
12. Commit to ensuring that community members affected by TB are engaged and participate fully in the development and implementation of TB policies and programming, including through financially and otherwise supporting TB prevention and treatment literacy campaigns and other community mobilisation efforts.
13. We call on Peter Sands, the Executive Director of the Global Fund to Fight Aids, Tuberculosis and Malaria to launch immediately a reprogramming and fundraising initiative to ensure high-TB burden countries modify their Global Fund-funded TB and TB-HIV programs to reflect the newest WHO treatment and prevention guidelines rather than old and outmoded approaches.
14. We call on the US Congress to urgently scale up funding for the President’s Emergency Plan for AIDS Relief (PEPFAR), the United States Agency for International Development (USAID), and Centers for Disease Control (CDC) to support expansion of life-saving TB and TB-HIV programming around the world, including by scaling up access to GeneXpert, aggressively expanding LAM testing, ensuring access to better and safer TB health technologies, and through funding the bold expansion of contact tracing and active case finding campaigns.
Issued by the Health Global Access Project, Global Tuberculosis Community Advisory Board, Global Coalition of TB Activists, International Treatment Preparedness Coalition, Kenya Legal & Ethical Issues Network on HIV and Aids (KELIN), Section27, Treatment Action Campaign, Treatment Action Group.
4:43 am 26 September: SA MPs sign up to fight for TB
Good morning, South Africa! The UN high-level meeting will kick off in less than 12 hours.
Until then, check out Speaker of the House Baleka Mbete reflect on former President Nelson Mandela’s bout of TB and what we should learn from it. Mbete is one of about 50 members of government who have signed onto become part of SA’s first TB caucus. They’ll form part of a global league of Parliamentarians who will help to make sure the goals in tomorrow’s declaration become reality. The club is the brainchild of Health Minister Aaron Motsoaledi and United Kingdom MP Nick Herbert.
Madiba developed TB during his time at Cape Town’s infamous Pollsmoor Prison. Decades later, the prison — like most correctional facilities — is still a breeding ground for infections.
David Bryden is the TB advocacy officer for the US non-profit Results. He explains why the international MP caucuses such as South Africa’s matter:
“Having this caucus is important because it gives civil society more points of contact in a country than just the health minister. Through it, you have access to some important influencers who can pass new laws but also make connections and brief high levels in the executive [branch of government]”, he says.
“For instance, you have a new TB law in the Philippines. With all the difficulties in a place like that, you have an energised parliamentarian who is able to get a law passed.”
The Philippines has been embroiled in a three-year “drug war”, which Human Rights Watch alleges has claimed at least 12 000 lives including those of human rights defenders and critics of the President Rodrigo Duterte’s repressive tactics.
So South Africa, meet your new TB caucus:
| Name |
House |
Constituency |
| Seiso Joel Mohai |
NCOP |
ANC Constituency: Springfontein (Free State) |
| Mzameni Richard Mdakane |
National Assembly |
ANC Constituency: Midrand (Gauteng) |
| Tebogo Josephine Mokwele |
NCOP |
EEF Constituency: Vryburg (North West) |
| Sheilla Xego |
| Jomo Nyambi |
National Assembly |
ANC Constituency: Naas (Mpumalanga) |
| Jackson Mthembu |
National Assembly |
ANC Constituency: Moses Mabhida Regional Office |
| Baleka Mbete |
National Assembly |
ANC Constituency: Kempton Park |
| Phoebe N Abraham-Ntantiso |
National Assembly |
| Anton Alberts |
National Assembly |
FF+ Constituency: Centurion (Gauteng) |
| Michael Bagraim |
National Assembly |
DA Constituency: Good Hope (Western Cape) |
| Maapi Angelina Molebatsi |
National Assembly |
ANC Constituency: Garankuwa (Gauteng) |
| James Mziwenkosi Mthethwa |
NCOP |
| Darren Bergman |
National Assembly |
DA Constituency: Centurion West (Gauteng) |
| Farhat Essack |
NCOP |
DA Constituency: Bushbuckridge, Thaba Chewu, Mbombela (Mpumalanga) |
| Archibold Figlan |
National Assembly |
DA Constituency: Drakenstein (Western Cape) |
| Prince Mangosuthu Buthelezi |
National Assembly |
| Narend Singh |
| Mkhuleko Hlengwa |
National Assembly |
| Liezl van der Merwe |
National Assembly |
| Jan Esterhuizen |
National Assembly |
| Xolani Ngwezi |
National Assembly |
| Ellen Prins |
NCOP |
ANC Constituency: Oudtshoorn (Western Cape) |
| Fezile Bhengu |
National Assembly |
ANC Constituency: Port St Johns (Eastern Cape) |
| Strike Michael Ralegoma |
National Assembly |
ANC Constituency: Ipelegeng/Dube (Gauteng) |
| Mergan Chetty |
NCOP |
DA Constituency: uMzinyathi (KwaZulu-Natal) |
| Steven M Jafta |
National Assembly |
AIC Constituency: Durban (KwaZulu-Natal) |
| Makoti Sibongile Khawula |
National Assembly |
EFF Constituency: Durban (KwaZulu-Natal) |
| Matthew Wolmarans |
National Assembly |
| Sibongile Nkomo |
National Assembly |
| Cameron Mackenzie |
National Assembly |
DA Constituency: Midrand West (Gauteng) |
| Steve Swart |
National Assembly |
ACDP Constituency: Free State |
| Motalane Monakedi |
NCOP |
| Sibusiso Christopher Mncwabe |
| Nthabiseng Khunou |
National Assembly |
ANC Constituency: Thaba Nchu (Free State |
| Moloko S. A. Maila |
National Assembly |
ANC Constituency: Senwabarwana (Limpopo) |
| Hildah Vangile Nyambi |
National Assembly |
ANC Constituency: Tonga |
| Nomsa Mtsweni |
MP Provincial Legis. |
ANC Constituency: Kwaggafontein (Mpumalanga) |
| Loyiso Mpumlwana |
National Assembly |
ANC Constituency: Umtata |
| Dikeledi Magadzi |
National Assembly |
ANC Constituency: Emalahleni |
| Nonhlanhla Ndaba |
National Assembly |
ANC Constituency: Katlehong (Gauteng) |
| Fish Mahlalela |
National Assembly |
ANC Constituency: Graskop |
| Malcolm Figg |
National Assembly |
DA Constituency: Tsitsi-Kouga (Eastern Cape) |
| Gerhardus Koornhof |
National Assembly |
ANC Constituency: Roodepoort (Gauteng) |
| Deidre Carter |
National Assembly |
COPE Constituency: KwaZulu-Natal |
| Mtikeni Patrick Sibande |
National Assembly |
ANC Constituency: Bethal |
| Madipoane R. M Mothapo |
National Assembly |
ANC Constituency: Mokgophong (Limpopo) |
| Xoliswa Tom |
National Assembly |
ANC Constituency: Middlerift (Eastern Cape) |
| Patrick Maesela |
National Assembly |
ANC Constituency: Evaton (Gauteng) |
| Gregory Allen Grootboom |
National Assembly |
DA Constituency: Diamond North, Diamond South |
| Aaron Motsoaledi |
National Assembly |
| T. Modise |
NCOP |
Speaker |
List courtesy of the TB/HIV Care Association
11:25 pm 25 September: Finally, hope for a new TB vaccine?
South Africa researchers may have solved one of the biggest questions standing between the world and a new TB vaccine, new research shows.
A new TB vaccine trial has been the first to show an almost 50% decrease in new TB cases, a study published Tuesday in the New England Medical Journal finds. The research was conducted among almost 3 580 adults in Zambia, Kenya and South Africa. As part of the trial, half were given a two-dose vaccine, and half received a placebo.
More than two years after getting their first dose of the vaccine, people who received the real vaccine were half as likely to develop active TB as those in the placebo group, according to the research conducted by TB research non-profit Aeras and pharmaceutical company GlaxoKlineSmith.
“[This] is really a game changer for this field”, Aeras Chief Medical Officer Ann Ginsberg explains.
“It’s really the first novel vaccine that has shown this level of efficacy. It’s also the first TB vaccine at all that’s shown you can protect people who are already infected with the bacteria but not yet sick.”
Everyone who took part had latent TB or had been infected with the bacteria.
While many people may carry latent TB, the active disease will usually only occur in a small number of people. However, those with compromised immune systems, such as people with HIV or diabetes, may as much as 30 times more likely to develop active TB, studies have shown.
David Lewinsohn is a professor of medicine at the United States’ Oregon Health and Science University and chairs the UN’s StopTB Partnership working group on new vaccines. He says that until now science hasn’t known very much about what separates healthy people who don’t develop active TB from those who do.
“It’s tackled the most difficult question in TB vaccinology, that is that most people who get infected do pretty well so it’s been a big open question as to whether you can improve upon natural immunity”, Lewinsohn explains.
“It’s a stunning result because it says we can, and even if this may or may not be the final answer, it really shows us the way forward.”
The study is expected to end in mid-2019 and was conducted in partnership with local bodies such the Medical Research Council and the University of the Witwatersrand. The research was not conducted among people living with HIV, an important group considering that the national health department has estimated that 60% of TB patients in the country are co-infected with HIV.
Although plans to confirm the findings are still being developed, Ginsberg says that testing whether it’s as effective among other groups, including HIV-positive people.
A small study to test the safety of the vaccine among people living with HIV and found the vaccine was as safe for HIV-positive people as those who were not HIV infected, she explains.
“It’s still going to be several years for sure [until the vaccine could be marketed if proven effective] but we’re eager to develop it as quickly as possible while still doing strong, robust studies.”
7:47 pm 25 September.
Funding TB has been one of the big issues in the run-up to tomorrow. Now, the advocacy organisation Treatment Action Group (TAG) has released new, preliminary figures on how much the world is investing to diagnose and treat TB.
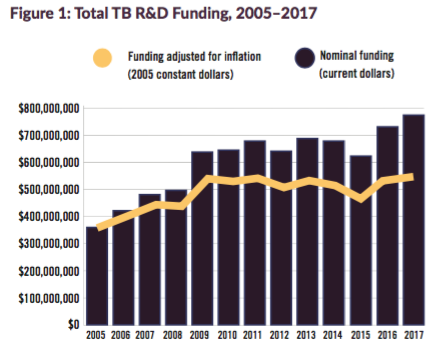
The bad news? Inflation means that in real terms, the level of TB R&D; spending is still at 2009 levels. Multiple outlets including The Lancet medical journal and Spotlight have said that tomorrow’s declaration will be meaningless without, in part, real increases in funding to back it.
The TAG report ends with a quote from Anele Yawa, secretary general of the Aids lobby group the Treatment Action Campaign:

5:06 pm 25 September: First things, first
First the basics. What is a UN high-level meeting? The gatherings are reserved for specific issues in exceptional circumstances. This is only the fifth high-level meeting on health issue ever so at this rate, we’ll have to wait another two decades for something similar.
Find out what to expect at the meeting in our latest analysis, including what didn’t make it into the final draft. In the meantime, here’s a quick summary:
| What’s left unsaid: Some of the others issues that didn’t make it into the final draft |
| 1. National targets, including specific goals for high-risk populations such as prisoners, miners or children |
| 2. Commitments to putting national targets on paper in the form of strategic plans |
| 3. Timelines for new innovations such as shorter, pill-based regimens for all forms of TB, rapid tests and vaccines |
| 4. An independent accountability mechanism outside the UN system — possible including the World Health Organisation — to ensure future engagements from heads of state |
| 5. National R&D funding targets. Dubbed the “Fair Shar Targets” this would have ensured that .1% of national research funding would have gone to TB |
Plus, check out this exclusive opinion piece with the man of the hour. Health Minister Aaron Motsoaledi, who is also the chairperson of the StopTB Partnership, banded together with his counterparts from countries like Brazil, Thailand and Senegal to hatch a plan to get the UN talking about TB. Today, his dream is a reality.
Why did it TB have to trail behind other diseases such as Ebola or HIV for its own high-level meeting? Here’s what he says:
Activists are also expecting some big announcements to coincide with the declaration’s release, including from the US government, which is a large funder of TB globally.
Read the final text of the declaration:
Note: Because of technical difficulties, some of the social media including in this post had to be re-loaded after the meeting.