Big Pharma is already showing signs of putting revenue ahead of saving lives in the race to find a Covid-19 vaccine, according to experts. (John McCann/M&G)
As the global race to find a safe and effective Covid-19 vaccine continues, concerns about pharmaceutical companies exploiting the pandemic to make profits are also rising. Activists and experts across the world fear that this industry, often referred to as “Big Pharma”, are already showing signs of prioritising revenue over equitable access to life-saving drugs.
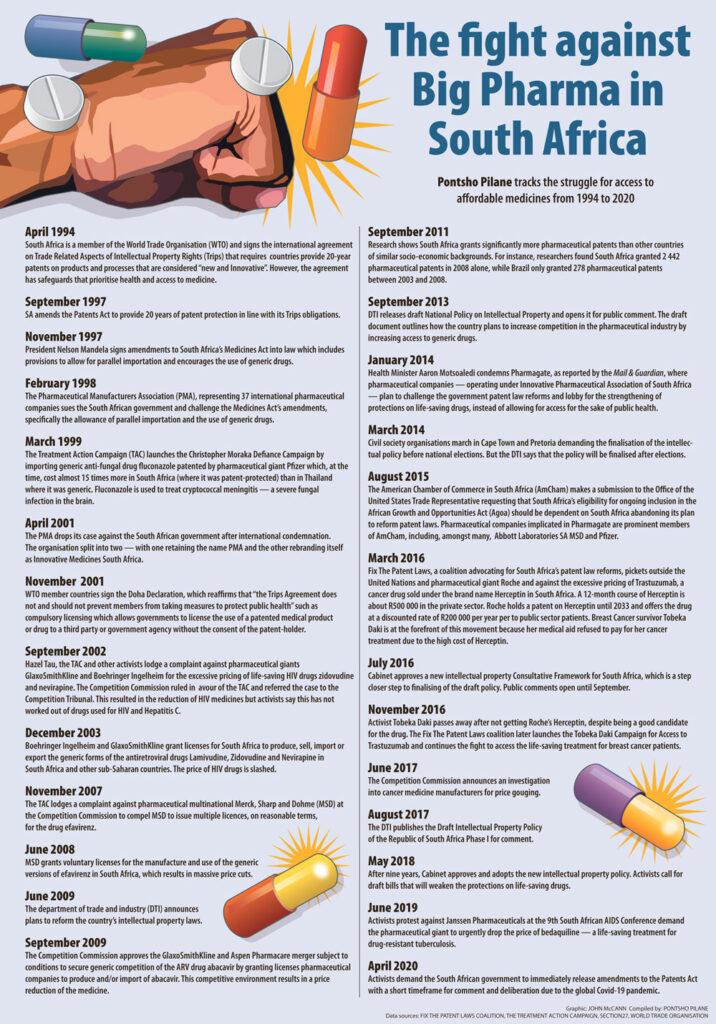
South African activists are concerned that the government is not proactive enough in ensuring the pharmaceutical industry doesn’t take advantage of the country’s intellectual property (IP) laws to benefit from the pandemic at the cost of people’s health and lives.
“It’s unusual because during the lockdown government has been pushing back against the tobacco and alcohol industries, and these are considered powerful industries and powerful lobbyists. It’s rather surprising that the most obvious industry — the pharmaceutical industry — that needs to be challenged head-on is not necessarily within government’s public focus,” Fatima Hassan says.
Hassan is a veteran human rights lawyer who litigated against the government and pharmaceutical companies for access to HIV treatment in the late 1990s and early 2000s for the Treatment Action Campaign while at the AIDS Law Project. She recently founded the Health Justice Initiative.
She believes the government has kept quiet about Big Pharma because there is a “very cosy relationship” between the South African government, the ANC and the pharmaceutical industry. “There are multiple vested interests, which need to be looked at, investigated and examined with both brand-name and generic drug companies,” Hassan says.
Pharmaceutical companies have previously tried to strong-arm the South African government into leaving our current patent laws in their favour.
In 2015, companies that were members of the American Chamber of Commerce in South Africa — including, among many, Abbott Laboratories SA, MSD and Pfizer — sent a request to the Office of the United States Trade Representative. The submission was for the representative to make South Africa’s inclusion in the African Growth and Opportunities Act contingent on the country abandoning its plan to reform patent laws.
Additionally, it took almost a decade for the cabinet to adopt the country’s IP policy, which, when implemented, can ensure that adequate treatment — for diseases such as Covid-19 — is affordable and accessible to those who need it.
However, the national department of health says it has been in meetings with relevant stakeholders about Covid-19 vaccines. Despite global supplies running thin, it is working with local and international companies to acquire all essential health products.
“Fortunately, the medicines currently recommended for use in the management of Covid-19 are already on contract, and also recommended for use for other conditions. The contractual terms concerning pricing bound the contracted suppliers,” says health department spokesperson, Popo Maja.
The ANC did not respond to Mail & Guardian’s query about its relationship with pharmaceutical companies and whether the political party has received any donations from any pharmaceutical companies in the past.
Will Big Pharma strike again?
Over the years, civil society organisations forced pharmaceutical companies to grant licences for lifesaving drugs — such as HIV medicine — through litigating against both the government and Big Pharma.
Lack of political will is the reason that activists have resorted to using the legal system as a means to get access to medicines for most South Africans, says Médecins Sans Frontières (MSF) South Africa’s access campaign advocacy officer, Candice Sehoma.
“It’s concerning that nothing much has happened in terms of expediting our patent laws to enable access to health products that could help in treating Covid-19 in the future. We have seen with our work with HIV, cancer and tuberculosis medicine that the current system allows for a company to be the sole manufacturer and have a monopoly on a specific health product. This also allows companies to price drugs as expensive as they please,” Sehoma says.
MSF South Africa and about 40 other organisations advocating for patent law reform in South Africa, are part of the Fix the Patent Law coalition. They are calling for the government to put a temporary moratorium on issuing patents on all Covid-19-related health products and to institute compulsory licensing — granting the government the power to give other pharmaceutical companies patent rights without the consent of the rights holder.
The coalition has called the country’s patent laws “outdated” and says they could curtail access to future Covid-19 treatments or vaccines.
According to the department of trade, industry and competition, there have been no Covid-19 related pharmaceutical patents granted to any pharmaceutical companies in South Africa, yet. The department, however, concedes that aspects of South Africa’s patent laws do have the potential to pose risks, and that this is an issue the government has been aware of even before the Covid-19 pandemic.
 (John McCann/M&G)
(John McCann/M&G)
The department’s legal director, Marumo Nkomo, says: “The IP policy [that cabinet approved in 2018] calls for various amendments to the Patents Act to ensure a more equitable balance between the interests of patent right holders and the public interest. Technical work to effect the reforms is at an advanced stage … and bringing South Africa’s compulsory licensing provisions in line with international best practices is among the patent reforms developed.”
More clinical trials a good sign
This week, South Africa signed up to two more Covid-19 clinical trials in the race to find viable immunisation. Clinical trials for the two vaccine candidates — Ad26.COV2-S and NVX-CoV2373-s — from pharmaceutical companies Johnson & Johnson and Novavax will begin next month. This follows the launch of the Ox1Cov-19 Vaccine Vida trial in June, which is a collaboration between Oxford University and the University of the Witwatersrand.
Health Minister Zweli Mkhize says participating in clinical trials positions the country favourably for when a vaccine becomes available to the market. “Countries that invested into the development of these tools through research and development tend to be prioritised when they go to market. However, we remain cognisant of the threat of shortage compromising access, not only for ourselves but for other countries,” he says.
Although there is currently no viable vaccine for Covid-19, concerns about vaccine hoarding intensified after the United States department of health and human services announced an agreement to purchase large quantities of the drug remdesivir with pharmaceutical giant Gilead. Remdesivir is one of the drugs that’s been tested as treatment for Covid-19 and the US Food and Drug Administration has approved emergency use of the drug during the pandemic. Various clinical trials — both in the past and ongoing — are investigating the efficacy of the medicine.
Meanwhile, the US has secured more than half a million treatment courses of the drug for US hospitals until September — which represented 100% of Gilead’s projected production for July, and 90% of production in August and September, as well as supply to all ongoing clinical trials involving remdesivir.
Gilead, however, signed non-exclusive voluntary licensing agreements with five pharmaceutical companies based in Egypt, India and Pakistan “to further expand the supply of remdesivir”. These licences cover distribution to 127 countries, including South Africa and several other African countries.
Although activists and experts across the world continue to raise concerns about the possible hoarding of future treatments and vaccines, the department of trade, industry and competition calls Gilead’s voluntary licensing agreements “another example of co-operation proving effective in practice”. The licenses allow the five generic pharmaceutical manufacturers to receive technology transfer on Gilead manufacturing processes and are royalty-free for the duration of the pandemic.
But the question remains: Will goodwill and co-operation from Big Pharma guarantee access to Covid-19 treatment and vaccinations when they hit the market?