Dr Llewellyn Volmink grew up in the township of Nkqubela in Robertson and is now a medical doctor working in the local hospital.
Early on a Saturday afternoon in Ladismith in the Little Karoo, just after lunchtime, Llewellyn Volmink’s little body stiffened when he heard the adults screaming in terror. The truck full of farmworkers had just arrived. They climbed from the vehicle in dribs and drabs, grocery bags in their hands.
It was time to begin the weekend with bellies full of food and wine. It was time to forget the week’s hard labour, and all of life’s many problems. The midsummer heat hung heavy in the air. The farm’s ostriches lay languidly under wooden shading.
Llewellyn had been sitting on the lawn in front of the home of his farmworker grandparents, eagerly eating a treat they’d bought him in town earlier that day. Ouma and Oupa were lounging on the stoep watching their four-year-old grandson, whom they regarded as their own son.
But it was in a split second that the peace ended. Earsplitting yells filled the air and adults ran around manically. The boy turned to see Oupa on the ground, blood gushing from his neck. A relative had stabbed him with a knife after a quarrel they’d had earlier that week. Ouma was hysterical.
The police came to arrest the suspect. Llewellyn watched as they bundled him into their vehicle.
An ambulance had been summoned, but it never arrived.
Llewellyn had a long time to stare at his grandfather’s crooked, blood-soaked body.
“And that was when I knew I wanted to become a doctor,” the 27-year-old Dr Llewellyn Volmink says, as he places a stethoscope to his ears to listen to an elderly patient’s breathing in Robertson Hospital, a public health facility in rural Western Cape.
 Dr Llewellyn Volmink with his grandmother Irene Lizwane
Dr Llewellyn Volmink with his grandmother Irene Lizwane
Mixed heritage
When Volmink began school, he moved to Robertson to be cared for by his paternal grandmother, Irene Lizwane, in the township of Nkqubela. His parents were separated and neither had the financial means to look after him. His mother was a domestic worker in Cape Town, three hours away from Robertson, and his father an assistant in a hotel kitchen.
Volmink stayed with Lizwane until he matriculated. The move, however, came with huge adjustments: his maternal grandparents, who were coloured, brought him up speaking Afrikaans; his paternal grandmother was Xhosa, like his father. Although he attended an Afrikaans school in Robertson, he lived in a Xhosa township with a Xhosa family.
“I had to learn to speak the language and to adopt Xhosa culture,” he remembers. “It was difficult, but today I can say I’m truly trilingual. I speak fluent Xhosa, Afrikaans and English.”
Twenty years later, his language abilities and medical skills mean Volmink is one of the most sought- after commodities in South African medicine: a doctor who is able to help most of his patients by communicating with them in their mother tongues. In Robertson, Afrikaans and Xhosa are spoken almost exclusively.
“It’s my role to explain to patients, in their own language, and like a lay person, what is wrong with them and how we’re going to help them,” Volmink says.
He hangs his stethoscope around his neck and makes an inscription in a patient’s file in the hospital’s female adult ward. Then he turns to the elderly coloured woman, who suffers from chronic obstructive pulmonary disease, which makes it hard for her to breathe, and asks: “Voel tannie beter vandag? Help die pompie? [Are you feeling better today, aunty? Is the inhaler helping?]” The woman responds: “Dankie, dokter. Ek gebruik hom presies soos jy gesê het ek moet [Thank you doctor. I use it exactly the way you told me to].”
Patients not served in their home
Only 6% of patients in a Western Cape teaching hospital said they could speak to doctors in their home language, according to a 2006 study published in the South African Medical Journal. Language and cultural barriers were cited by more patients as a “major barrier to healthcare” than long waiting hours or the cost of transportation to and from health facilities.
State patients not competent in English – the language most South African doctors use to communicate with patients – are “less likely to have a regular source of primary care and are less likely to receive preventive care”, according to the 2012/2013 South African Health Review. They’re also at an “increased risk of experiencing medical errors”.
Volmink moves on to a patient on the opposite side of the hospital room and opens her file. “Uziva ka-njani emva kwayizolo? [How are you feeling after last night?]” he asks the woman, who had been vomiting the previous night.
“Ndiziva ndityhafile gqirha, kwaye ndinxaniwe gqirha. Ndicela undiphe amanzi? [I feel weak and thirsty, doctor. Could you please give me some water?]” she replies.
“I’m the only doctor at my hospital who understands Xhosa, so when a Xhosa patient arrives, I get called, because they are able to explain to me in the language they are most comfortable with why they’ve come to the hospital,” Volmink explains while pouring water into a glass for his patient. “It makes it easier for us to help them. We provide a much better service when we communicate with them in their home language.”
 Dr Llewellyn Volmink works at Robertson Hospital in the Western Cape
Dr Llewellyn Volmink works at Robertson Hospital in the Western Cape
Not enough doctors
All around the world, doctors based in rural districts are rare. According to the World Health Organisation (WHO), 46% of South Africa’s population live in rural areas but only 12% of the country’s physicians work there.
Research by the Rural Health Advocacy project at the University of the Witwatersrand indicates that, in rural areas, there are only 13 general practitioners and two specialists available for every 100 000 people without medical aid, compared with the national average of 30 doctors and 30 specialists per 100 000 people.
That’s despite the fact that, according to a 2009 study published in the health journal Rural and Remote Health, people living in rural areas are, on average, sicker and poorer than people in urban areas. The WHO argues that, because they tend to suffer more intense illness, rural populations actually need a proportionately higher number of doctors than city dwellers.
For instance, Volmink’s health district, the Cape Winelands, which is mainly rural, has the highest percentage of children under five in the country who suffer from diarrhoea (and consequent dehydration) and significantly more people here have tuberculosis than the national average, according to the 2013-2014 South African Health Review.
Various studies have shown that doctors are reluctant to work in rural areas because, among other factors, it’s difficult for them to build families in isolated districts owing to insufficient infrastructure and accommodation and inferior schools.
Reversing the trend
But doctors who grew up in rural areas, like Volmink, are helping to reverse this trend. According to a 2009 Cochrane systematic review, internationally recognised as the highest standard in evidence-based healthcare research, the single most important factor associated with a physician practising medicine in a rural area is when the doctor grew up in such a district.
Several international studies show that medical graduates raised in rural areas are far more likely to return to practise in such areas than their urban counterparts. In South Africa, the WHO reports that medical students from a rural background are three times more likely to practise in a rural location.
At Stellenbosch University, where Volmink studied, 10% of the medical school’s intake comes from rural towns. Volmink, who is completing his year of community service after graduating in 2011, didn’t return to just any rural district. He purposefully returned to his hometown and plans to practise medicine in Robertson for “at least a few more years”.
He explains: “I missed my grandmother; she’s getting old and is starting to show signs of dementia. I wanted to be close to her. But more than that, by being a doctor here I wanted to give something back to the community and return to my roots in Nkqubela. I now stay here again and it’s where I feel safe.”
 Dr Llewellyn Volmink services his patients in their home languages
Dr Llewellyn Volmink services his patients in their home languages
Rural training helps to develop rural doctors
In 2011, Stellenbosch University opened South Africa’s first rural clinical school, based in Worcester, about 100km from its main medical campus at Tygerberg Hospital in Bellville, Cape Town.
Studies in the United States, New Zealand, Australia, China and the Democratic Republic of the Congo have revealed that exposure to rural areas during undergraduate studies influences health workers’ subsequent choices to practise in those areas – even for students with an urban background.
The Australian government has taken this situation so seriously that it requires most public medical schools to ensure that at least a quarter of students undertake their studies in a rural setting for at least 12 months.
Since 2012, Stellenbosch University’s Ukwanda Rural Clinic School has allocated about 20 full- time spaces to the annual intake of medical students to spend their last year of studies, which consists of a supervised student internship, at Worcester Hospital, a regional hospital, or in one of the other rural district hospitals in the area. This is in stark contrast with the other 160 students who complete their studies at Tygerberg Hospital, which is a tertiary institution.
Volmink was one of Ukwanda’s first eight students in 2011. In 2006 he received the first provincial health department bursary allocated to a Stellenbosch University medical student from a rural background.
Better learning environment
“The fact that Uwkanda specialised in rural medicine wasn’t my only consideration when choosing to spend my last study year in Worcester. It was also a much better learning environment than Tygerberg, as there was more supervision and more opportunities to learn clinical skills,” Volmink says.
According to Ukwanda’s director, Hoffie Conradie, the student-tutor ratio during rotations at Worcester Hospital is often as low as two students to one consultant specialist, compared with a ratio 10 times that at Tygerberg.
“Students’ experience in this setting is that they become much more part of the team and directly involved in patients. Their feedback is that their transition from being a student to an intern doctor [after graduating] was much easier for them because they already worked like that,” says Conradie.
Ukwanda’s first students are now doing their year of community service. Seven of the eight students have chosen to do their service year in a rural area, including some from urban backgrounds.
Volmink maintains that he and his fellow Ukwanda students were exposed to patients with a “disease profile far more representative of South Africa’s burden of disease” than their Tygerberg colleagues.
“We saw patients at entry level, because we worked at regional and district hospitals. So we got a lot of experience with HIV, tuberculosis and lifestyle diseases,” he says. “Our Tygerberg colleagues worked at a tertiary institution, where only patients requiring specialised care are referred.”
Conradie explains: “The real test of our success rate of producing rural doctors through exposing them to a rural clinical year will be when their community service year is completed. We will then be able to start tracking who stayed on in a rural area, particularly at a public health facility, in the long term.”
He believes this will contribute important information to the South African health system, and allow for better planning of future healthcare strategies.
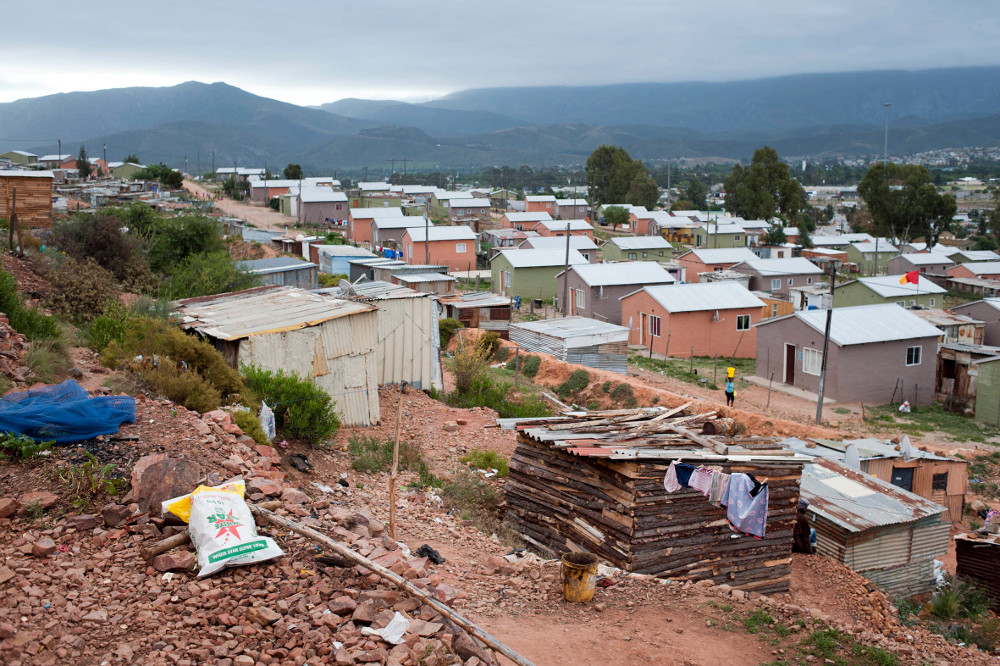 Home: Dr Llewellyn Volmink grew up in the township of Nkqubela in Robertson
Home: Dr Llewellyn Volmink grew up in the township of Nkqubela in Robertson
Against the odds
As a boy, Volmink wasn’t alone in his conviction that he was destined for the medical world: in Grade 2, his teacher was so persuaded that she gave him the nickname of “Doctor”.
“Doctor” was different from his peers. He read with remarkable ease and mathematics and other subjects came easily to him – so much so that, when he didn’t get full marks for school tests, his teacher would be upset. “She would pinch my neck,” Volmink recalls, with a wry smile.
But “Doctor” was not set apart from his peers in at least one aspect: he lived in extreme poverty.
Lizwane looked after her three grandchildren on a state pension of R400 a month. Volmink’s father had six children; all but two with different mothers. There were a lot of mouths to feed. Volmink’s biological mother stopped making contact with him soon after he moved in with his grandmother.
He recalls: “There was no money for school shoes. In the winter we used to wet our feet before we started walking to the bus, otherwise it took hours to get the sensation back in your feet. I have no idea what the logic behind it was, but it worked.”
The government high school he attended in Robertson was poorly resourced and wracked by violence. “It was the norm there to be part of a gang. Kids stabbing each other on the school grounds was common,” says Volmink.
Children from Langeberg Secondary School didn’t become doctors. If they were lucky, they got employment as general workers in the town’s retail stores, or as farm or construction labourers.
From the beginning, the odds were stacked against Volmink achieving his dream.
WHO research says most medical students from rural areas struggle to finance their studies, as their families’ incomes are usually much lower than those from urban regions.
The WHO’s 2010 global policy recommendations for increasing access to health workers in rural areas emphasise that such students don’t only need more financial assistance than urban students, but also significantly more academic and social support.
Despite his circumstances, Volmink obtained a 78% average in matric – a result that enabled him to be accepted into medical school. But although his Western Cape health department bursary paid for his studies, Volmink faced far more challenges than financial tribulations. “I felt extremely intimidated and inadequate,” he explains. “Almost all the other students were from model C schools. They had so much pedigree. I was just a rural township boy who didn’t think he’d pass. [At the time] no one in my family had ever been to university, so I had to figure out ways on my own to overcome my insecurities. Studying intensely and excessively was one such strategy.” According to Conradie, Stellenbosch has an “extended degree programme” for medical students who come from poorly resourced schools. It allows them two years to complete their first year of study. But Volmink wasn’t accustomed to life’s easier routes. After all, they’d never yet revealed themselves to him. Says Conradie: “Volmink chose to follow the main programme. And he never failed a subject.”
 Dr Llewellyn Volmink works at Robertson Hospital in the Western Cape. Last month, his son Llewellyn Junior was born in the same hospital
Dr Llewellyn Volmink works at Robertson Hospital in the Western Cape. Last month, his son Llewellyn Junior was born in the same hospital
His son’s personal doctor
On a humid morning in mid-October, Volmink rushed to Robertson Hospital. A woman’s baby was a week overdue but still there was no sign of the child being on its way into the world. A sonar scan revealed the infant’s umbilical cord was caught around his neck; an induced natural birth was considered too dangerous.
The medical team, of which Volmink was part, decided on an emergency procedure. But he didn’t want to perform it himself. He was unnerved by it. Although Volmink had completed several emergency caesarean sections in the past, this one would be different. So he handed the scalpel to one of his colleagues.
Volmink gazed out of a window. A soft drizzle had started to fall. Inside the young doctor, a distant part of his Xhosa culture stirred: “Rain brings blessings,” he thought.
His teammate began cutting into the woman’s abdomen. When Llewellyn Volmink junior gave his first cry at 11.25 that morning and threw his little arms up in the air, Dr Volmink dropped his camera. Joy had overwhelmed him.
“It was a boy with my face, mouth and eyes. A mini-me,” he smiles.
A few days later he took his son home, to the RDP house in Nkqubela that he rents from his grandmother for his family. He pledged: “My son will know where money comes from, and how hard it is to get it.”
After paternity leave, Volmink returned to work. His first patient was a five-year-old boy suffering an asthma attack. The boy was wheezing. Volmink began thinking of his own son, of all the trials and triumphs, the illnesses and happiness that lay ahead of Llewellyn Junior.
Then the doctor seated himself next to the young patient and his concerned mother, and said: “Yiza ndikubonise ukuba isebenza njani inqawe yesifuba. Kubalulekile ukuba uyisebenzise ukuba ufuna ukuphila impilo eqaqambileyo [Let me show you how the inhaler works. It’s very important that you use it if you want to stay healthy].”
After the consultation, Volmink made another promise to himself. “I’ll raise my son in a rural town where it’s still safe to run and play in the streets. And when he falls ill, I’ll be his own personal doctor.”
[This story was originally published on 21 November 2014]
