South Africa may still need donor support to fund expanded ARV roll out in the country.
South Africa’s HIV budget would have to increase by 50% to 60% in the next five years to total about R35-billion a year by 2020 if the country is to provide treatment for everyone with HIV and reach United Nations targets.
This is the finding of one scenario in the health department’s HIV and tuberculosis (TB) investment case published in March.
In September, the country will implement World Health Organisation guidelines, which recommend that all people with HIV should be on lifelong treatment regardless of their CD4 count, which is used to measure the immune’s system’s strength. Currently, most HIV-positive people in South Africa must wait until their CD4 counts fall to 500 to access antiretrovirals (ARVs).
By the end of March, 3.4-million people were on treatment, but South Africa has 6.8-million people with HIV, according to health department data. The number of people on ARVs would have to double to meet the new guidelines.
Treasury data show that the country’s conditional grant for HIV has grown from R1-billion since its introduction in 2003/2004 to R15.3-million in 2016. This is likely to reach R20-billion by 2018/2019.
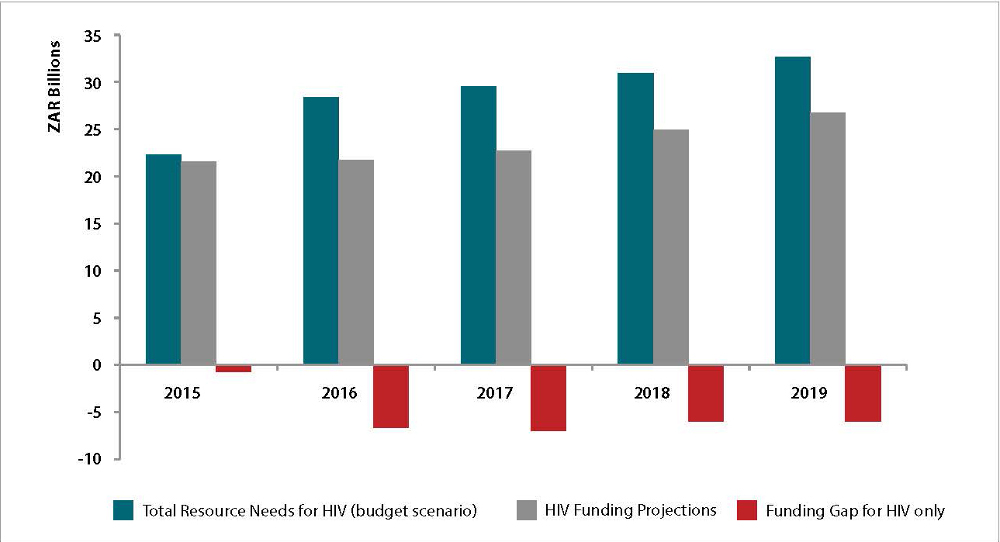
The total costs of South Africa’s HIV programme are expected to outstrip projected domestic funding in the next three years, leading to funding gaps. (Source: South Africa’s HIV and TB investment case)
South Africa is one of the few developing countries that carries the bulk of the cost of its HIV programme.
Speaking at a high-level panel at the Durban International Aids Conference earlier this week, the treasury’s chief director for health and social development, Mark Blecher, said the government has “consciously chosen to fund over 80% to 85% of the epidemic, or multiple epidemics, with domestic public funds because it’s our duty and responsibility as government to do so”.
“General taxation continues to be the most important source of financing,” he said. “Despite the fact that South Africa is currently experiencing a period of significant fiscal constraints government will continue to prioritise HIV and TB.”
The investment case projects that the portion of HIV funds covered by the government will continue to rise, but there is likely to be a substantial “resource gap” for each year in the next five years.
Health Minister Aaron Motsoaledi said one of the ways to pay for the increased demand in treatment is for the government to negotiate cheaper prices for the medicine.
“If we calculated the amount of money that was going to be needed, based on 2002 estimates, to put 3.4-million people on treatment, it would have added up to around R40-billion,” he said.
“But that did not happen because we were able to negotiate a more than 50% drop in the price of ARVs per patients to R314 per month. Soon after that we introduced the fixed-dose combination [ARV] and the cost went down to R89, meaning that we could double the number of patients without getting more money from treasury.”
South Africa has two main donors, the Global Fund to Fight Aids, TB and Malaria and the United States President’s Emergency Plan for Aids Relief (Pepfar), which assist it to fill financial gaps in its HIV programme.
Pepfar has focused its donor funding in South Africa on population groups and areas with the highest HIV infection rates.
The US government’s global Aids co-ordinator, Deborah Birx, said: “We should be making sure that the dollars have maximum impact by coordinating with the government and the Global Fund and any other bilateral donor.
“This is not the time to withdraw funding; this is the time to support South Africa to end its epidemic.”