Mortality: An attendant at Avbob in Pretoria waits for the coffin of a patient who died of illness related to Covid-19. The pandemic has, so far, claimed the lives of 54 237 South Africans. (Marco Longari/AFP)
Friday, April 30, marks day 400 since South Africa was placed under a national state of disaster caused by the Covid-19 pandemic.
Just over a year later, the country has recorded more than 1.5-million infections and 54 237 Covid-19 related deaths. Hit hard by the second wave of infections at the start of the year — a third wave is expected, while South Africa is administering vaccines at a rate slowed by setbacks.
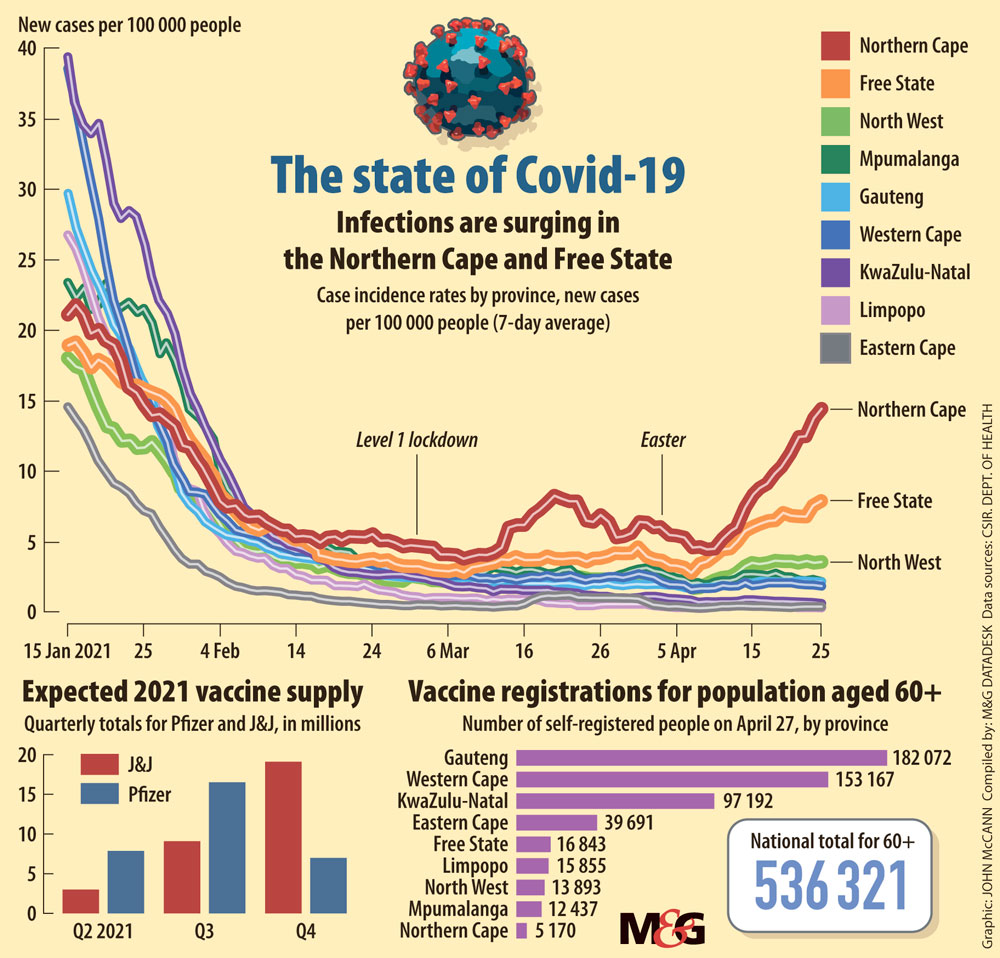
According to the Council for Scientific and Industrial Research’s Dr Ridhwaan Suliman, the Northern Cape is currently the most significant cause for concern. New cases in the province have reached a three-month high — shooting up almost immediately after the April Easter break finished. The Free State has followed an almost identical trajectory.
Although not in the same alert bracket, North West has some red flags. The rise in cases registered here has “failed to fall” since the middle of the month, according to Suliman.
The Northern Cape incidence rate is more than 60% — doubling every 10 days, representing 64% of its second wave peak. The Free State increase is 23% up, week-on-week, with case incidence at 41% of its second wave peak.
Suliman said all other provinces were stable, with curves flat-lining this week.
Similar data was presented to the parliamentary portfolio committee on health on Wednesday.
Briefing the committee, health director general Sandile Buthelezi said a gradual increase in Covid-19 infections since February might imply a potential resurgence, depending on factors such as contact rates increasing during holiday periods.
According to the department’s presentation to parliament, the Northern Cape has the highest number of active cases per 100 000 population at 256.3. The Free State follows with 102.3, North West with 66.7; KwaZulu-Natal with 44.4 and the Western Cape with 28.7.
“The timing of the third wave is uncertain due to uncertainty in the rate at which contacts increase,” said Buthelezi
He said the time from the initial increase in transmission until reaching a peak is, on average, two to three months, based on data.
If South Africa is recording a gradual increase since February, a possible peak should, or must soon, be noticeable. Instead, the opposite is shown in the data.
“Nationally, there has been a 16.9% decrease in new cases compared to seven days prior [to Monday 26 April]. Five provinces showed positive percentage changes,” said Buthelezi, adding that “there has been a 12.7% decrease in hospitalisations” compared with seven days before Monday.
Although the country shows a 0.05% increase in new Covid-19 cases since its latest report on 27 April, nationally the number of recoveries increased by 0.05%, representing a recovery rate of 95.3%. There are 20 254 active cases in the country.
The data also shows that nationally, as of 26 April, there has been a 12.7% decrease in admissions to hospitals when compared with the previous week. But six provinces showed increases in admissions — Eastern Cape, Free State, Limpopo, Mpumalanga, Northern Cape and North West.
“The upward trajectories in hospitalisations, positivity rate and new cases observed in the Free State, Mpumalanga, North West and Northern Cape are of concern and will be monitored closely.
“The Free State currently reports the highest number of hospitalised patients per 100 000 population at 12.9, followed by the Western Cape at 10.4; Northern Cape 8.7 the North West at 8.4; Gauteng at 8.2; KwaZulu-Natal at 3.9 and Mpumalanga 3.7,” reads the presentation.
With Covid-19 infections gradually increasing and South Africa’s winter approaching, the rollout of vaccines is crucial in the battle against Covid-19.
As of Tuesday, 27 April, just more than 1.3-million people had registered to receive a vaccination. Of these, more than 804 000 are healthcare workers and half a million people are over the age of 60.
Of these, 292 623 vaccines had been administered by 19 April before the vaccination programme was temporarily suspended, which was the second setback for the vaccination programme.
 (John McCann/M&G)
(John McCann/M&G)
The suspension, which ended on Wednesday, came after about 13 people in Europe and the United States died after an immune thrombotic thrombocytopenia event, a blood-clotting disorder. Although there were no such local deaths, Health Minister Zweli Mkhize suspended vaccinations in line with several European countries and the US.
The first delay occurred in February, when the one-million vials AstraZeneca vaccine rollout was halted because of low efficacy against mild and moderate cases of the 501Y.V2 variant. This consignment was sold to the African Union, which distributed it to other countries, including Nigeria, Ghana, Egypt and Zimbabwe.
South Africa waited two weeks for the Johnson & Johnson consignment to arrive to vaccinate healthcare workers.
The portfolio committee on health’s Kenneth Jacobs told the department of health during Wednesday’s meeting that there “is a general concern with the pace of vaccine rollout in South Africa, especially considering that we have 880 new cases in the past 24 hours.
“There is increased hospitalisation in certain provinces, although there is a national decrease. People generally have a concern with a third wave coming sooner than expected, and that we know that there are no new variants in South Africa, but we know that variants may merge at any time.”
Lucille Blumberg, deputy director at the National Institute for Communicable Disease (NICD), told the Mail & Guardian that there is an increased probability of a mid-May infection surge.
She attributes this to church and social events during the April holidays. These could have sparked some “super-spreader” events, which could push the spread to critical levels.
“People let down their guard. It’s nothing new,” she added.
Nationally, as of 26 April, there has been an increase of 8.9% in the number of deaths compared with seven days prior.
Though a significant concern, the department said that in the absence of a new variant, the experts expect the peak of the third wave to be lower than the second wave.
“In all age groups, the hospital admissions are projected to be lower than levels in the second wave,” reported the department.
Blumberg said it takes a little time for the coronavirus to circulate to reach a critical level and then cause enough infection to affect the hospital system.
“For the over 60s, I don’t think the vaccinations will impact — it will all depend on how fast you roll it out, how many people you reach and how effective the vaccine is. The vaccine may not prevent transmission and mild infection, but it will prevent death and severe illness,” she said.
The importance of vaccinating those older than 60 is illustrated by NICD mortality and hospital admissions statistics. People of 60 and older account for 60% of hospital admissions and 32% of deaths.
But the Sisonke vaccination programme has restarted and will now certainly overlap with the wider phase 2 rollout scheduled for 17 May.
Both the minister and Buthelezi were confident that the second phase would begin on time.